Peri-implant disease: Treatment
As with periodontitis, peri-implant mucositis and peri-implantitis develop as a result of the accumulation of bacterial plaque. So, the treatment for these two implant diseases adopts the same principles of therapy as those used in treating gingivitis and periodontitis.
There are several levels of treatment depending on the level of the disease around the implant.
Peri-implant mucositis
Like gingivitis, peri-implant mucositis is prevented and treated by good oral hygiene and by professional cleaning, which should be done at least twice a year.
Patients who have lost teeth because of periodontitis should keep in mind that implants are less resistant to the development and progression of disease than teeth. This means that implants need to be carefully monitored to prevent problems around implants or to stop them at an early stage.
Peri-implantitis
If peri-implant mucositis progresses and turns into peri-implantitis several approaches, depending on the severity of the bone loss around the implant, can be adopted.
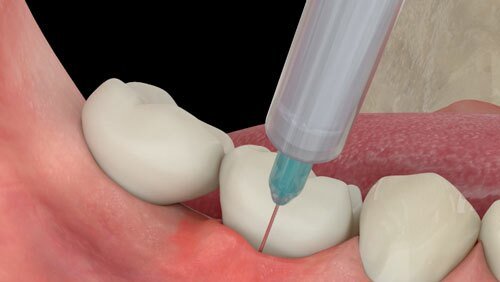
- The first step in treating peri-implantitis (as in periodontitis) is professional non-surgical therapy together with the use of chlorhexidine mouthwashes and gels to decrease the number of bacterial deposits.
- It is also important that the dentist or periodontist checks to see if there are any deposits of cement (from when the crowns were cemented to the implants) beneath the gums and around the implant. This factor is often associated with the development of peri-implantitis.
- At re-evaluation, usually after six weeks, if the bleeding has stopped or decreased and if the probing depths (the depth of the “pockets” around the implant measured by the periodontal probe) have also decreased, recall appointments are scheduled according to the professional’s assessment of each patient’s needs.
- If there is significant bone loss with bleeding and pus that has not been resolved by the non-surgical therapy, various forms of treatment can be adopted. However, non-surgical treatment should first be repeated to control the bleeding and inflammation.
- Antibiotics: in some cases, following non-surgical treatment, antibiotics may be given to help control the infection before other treatments are tried.
- Once the inflammation around the implant has been controlled, if the problem requires surgical treatment the dentist or periodontist will decide which approach to use. This will depend on the nature of the damage caused by peri-implantitis. First, the gums are raised so that the defect can be inspected and then, depending on the circumstances, the options include:
- Bone regeneration using bone grafts.
- Resective surgery, which removes bony ledges and flattens the bone irregularities around the implant.
- Implantoplasty, where the threads on the screw of the implant are removed to leave a polished implant surface.
In fact, when treating peri-implantitis there is usually a combination of these different procedures.
It is of great importance that the gum around the implant is thick and non-mobile (“keratinised”), as this has been shown to prevent and decrease bone loss around the implants.
In many peri-implantitis cases, there is a lack of proper soft tissue around the implants. This can be corrected using various techniques, of which the most common is using grafts taken from the patient’s palate. Recently, collagen-based grafts derived from animals have been used as an alternative way to reconstruct the soft tissues around implants.
All this means that many steps are required to treat peri-implantitis, return a patient to peri-implant health, and prolong the life of an implant. Some cases will require only non-surgical therapy while others will need additional treatment.
The earlier that peri-implant mucositis and peri-implantitis are detected, the better are the chances of successful treatment.
But better still is preventing disease in the first place, through correct oral hygiene and regular professional cleaning of teeth, implants, and gums.