Frequently asked questions
What is periodontal disease?
Periodontal diseases – gingivitis and periodontitis – are the most prevalent inflammatory diseases among humans. Periodontitis, which is more severe than gingivitis, involves damage of the gums, bones, and other tissues that support the teeth. It is provoked by pathogens in dental plaque both above and below the level of the gums. In Western countries, periodontitis affects more than half of the population and around the world 750 million people suffer from severe forms of the disease.
What are the effects of periodontal disease?
If left untreated, periodontitis can cause tooth loss, which in turn can lead to problems with eating and speaking, aesthetic damage to the smile, and lower self-confidence and quality of life. Periodontitis is associated not only with a greater risk of diabetes (see below) but also with a higher risk of suffering from other conditions including cardiovascular disease, Alzheimer’s disease, certain forms of cancer, complications during pregnancy, and erectile dysfunction.
What is diabetes?
Diabetes mellitus (usually referred to simply as “diabetes”) is defined by hyperglycaemia (high blood-sugar levels) and has two major forms. Type I diabetes mellitus results from a lack of insulin because of an autoimmune reaction in the pancreas, whereas type 2 diabetes mellitus occurs as a consequence of insulin resistance associated with chronically high blood-sugar levels. There is now a global epidemic of diabetes, with one in 11 adults (415 million people) across the world suffering from the disease, the majority (about 90%) from diabetes type 2. In 2017, about 4 million people died as a result of diabetes. There are an estimated 212 million people worldwide with undiagnosed diabetes.
What are the complications of diabetes?
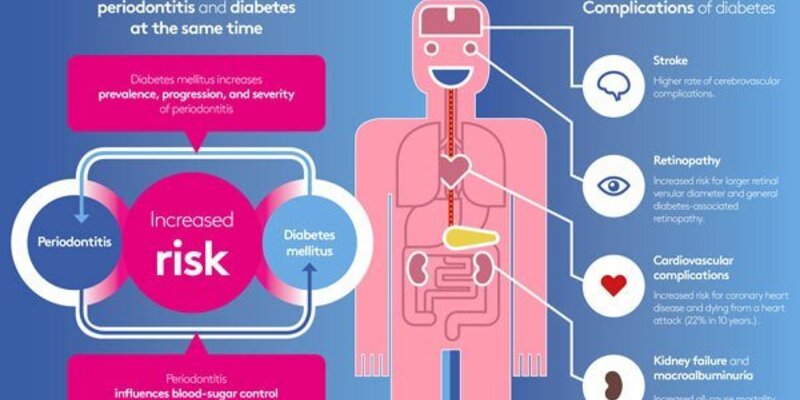
High blood-sugar levels over a long period of time can seriously damage blood vessels, which can lead to problems in different parts of the body. People with diabetes are at greater risk of suffering heart attacks, strokes, eye problems (retinopathy), kidney problems, and foot problems that can result in amputation.
What is the relationship between gum disease and diabetes?
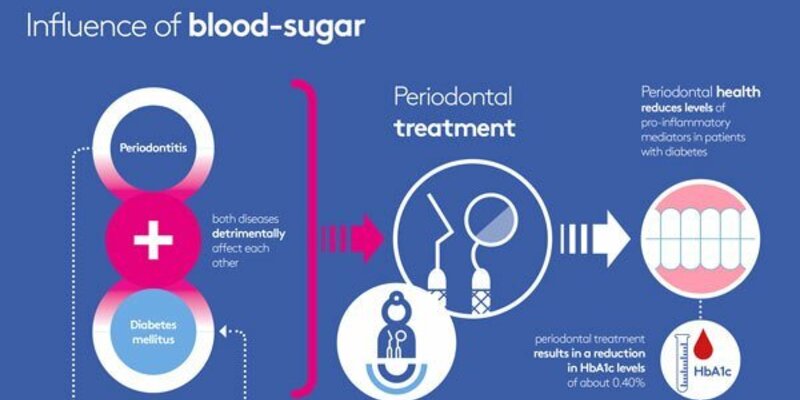
There is a bidirectional (two-way) relationship between periodontitis and diabetes. This means that healthy patients with periodontitis have a higher chance of developing pre-diabetes and diabetes, while people with severe periodontitis have an increased risk of developing type 2 diabetes. Periodontitis is significantly associated with poorer glycaemic control (HbA1c) and higher blood-glucose levels (glycaemia) both in people with diabetes and in those without the disease. There are higher levels of insulin resistance in people with periodontitis. Diabetes increases the risk of suffering periodontitis and it also increases the risk of the progression and severity of the disease. However, when periodontitis is successfully treated it may help improve a patient’s diabetes. Periodontal treatment in people with diabetes results in a significant reduction in HbA1c levels three months after periodontal therapy.
What happens if you have both periodontitis and diabetes at the same time?
Controlling diabetes is more complicated when a patient also has periodontitis. People who have both diabetes and periodontitis are at greater risk of suffering from certain severe medical complications – including heart disease, chronic kidney disease, and retinopathy – than people who have diabetes alone.
If I have diabetes, what do I need to do?
If your doctor has told you that you have diabetes, you should make an appointment with a dentist. Provide your dentist with an update of the results of your diabetes control and any changes in medication. Your dentist will give you personalised advice on what you need to do. Even if you do not have gum disease, you should still get regular dental check-ups as part of managing your diabetes. It is important to keep your mouth and body as healthy as possible with regular dental and medical care. And it is important to follow some basic oral-hygiene rules (clean your teeth and gums twice a day and use interdental brushes) as well as control of your weight, avoid smoking, and eat healthy foods.
I don't have diabetes, but I do have periodontal disease. What do I need to know, what do I need to do?
If you have periodontal disease, you have a greater likelihood of developing diabetes. In addition to visiting your dentist or periodontist to treat your periodontal disease, you should adopt a healthy lifestyle in terms of weight control, diet, exercise, and avoiding smoking, which will help prevent both diabetes and periodontal disease. Visit your physician regularly in order to screen the risk of incipient diabetes..
What do doctors and dentists need to do?
The prevention, early diagnosis and co-management between dentists and physicians of diabetes and periodontitis is of utmost importance. Physicians and other medical professionals are encouraged to follow the IDF/EFP “4Rs” guidelines (Recommend, Request, Refer, Recall). These guidelines include:
- Providing oral-health education to all patients with diabetes,
- Informing them of the negative impact of periodontitis on their overall health and their diabetes management,
- Letting them know how periodontitis increases risks of diabetes complications and mortality, and
- Explaining how successful periodontal therapy can have a positive impact on their health and well-being.
Physicians should always ask their patients about prior diagnosis of periodontal disease and about any signs or symptoms of periodontitis. They should ensure that the required periodontal care and maintenance are provided, referring patients to dentists where appropriate. All patients with newly diagnosed diabetes mellitus should receive a periodontal examination. Patients with diabetes have an increased risk of oral fungal infections and should be informed about this and treated if required.
Dentists and other oral-healthcare professionals are encouraged to compile a careful history from their patients who have diabetes, ask them how well controlled their diabetes is and when their blood-glucose levels were last checked, and request a copy of their most recent HbA1c results. A thorough oral examination should be carried out, comprising periodontal evaluation, full-mouth pocket chart, and bleeding scores. Oral-health education should be provided, together with individualised advice on risk factors and a tailored oral regime. Diabetes patients without periodontitis should be placed on a preventive care regime and monitored regularly, while those with periodontal infections should be treated and periodontal therapy provided.
Dental patients without diabetes but with risk factors for type 2 diabetes should be informed of their risk and referred to a physician for risk assessment and screening.
Physicians and dentists should collaborate in managing diabetes before any oral interventions or oral surgery.