![]()
3 December 2015
Podcast of Prevention Workshop webinar is now available for viewing
Category:Communication
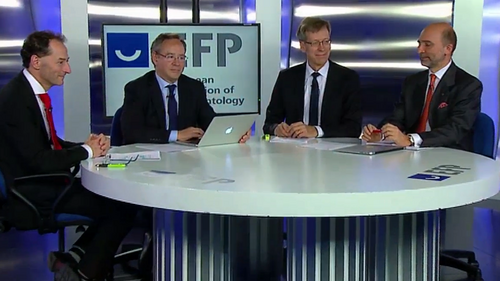
The podcast recording of the November 9 Prevention Workshop webinar – in which the four co-chairmen explained guidelines to prevent periodontal disease and peri-implantitis – is now available for viewing.
The online seminar, which was watched live by 420 viewers in 28 countries, was streamed live from a Madrid TV studio. It featured both informative videos and discussions between Mariano Sanz, Maurizio Tonetti, Iain Chapple, and Søren Jepsen about the conclusions and guidelines of the XI European Workshop in Periodontology, the Prevention Workshop.
“The outcomes of this workshop are fundamental for professionals and also for the periodontal and peri-implant health of our population,” said Prof Sanz, the chairman of the Prevention Workshop, in his introductory remarks.
The webinar covered all the key areas analysed by the Workshop, dedicated to 'Effective prevention of periodontal and peri-implant diseases,’ which took place in Spain in November 2014.
One of the biggest challenges highlighted by the four co-chairmen was changing the behavioural habits of patients at risk of periodontal or peri-implant diseases.
Prof Sanz highlighted the difficulties involved in assessing the susceptibility of patients, which “varies a lot”. He said there was a need for effective recall programmes so that patients could be continually re-assessed, as factors such as stress could affect their susceptibility.
Prof Tonetti, who chaired the Prevention Workshop’s working group on the principles of prevention in periodontal diseases, said that there were 750 million people around the world with periodontitis severe enough to put their teeth at risk of loss, an “incredible number”.
He said that while it was not yet possible to identify individual risk factors, it was possible to use risk-assessment approaches to assess segments of the population with different levels of risk of tooth loss. Prevention approaches needed to vary for the different patient groups: those with healthy gums, those with gingivitis, and those with periodontitis.
He added that patient compliance with oral-hygiene instructions was “the biggest challenge”, a point echoed by Prof Chapple, who pointed out that some patients need to devote 10-20 minutes twice a day to mechanical plaque control, and those that require longer hygiene times to maintain health might struggle to find that time and to reconcile this need with their busy lifestyles.
Chapple, who chaired the working group on the primary prevention of periodontitis, assessed various aspects of mechanical plaque control. While both manual and electric brushes were effective, rechargeable power brushes were “significantly more effective” than battery-powered brushes in reducing plaque scores and gingival inflammation. There was also a small but significant difference between power and manual brushing in favour of the former.
He emphasised the Workshop’s finding on flossing. “Perhaps what surprised most people was that there is really insufficient evidence to demonstrate that the use of dental floss offered any significant benefit for patients with gingivitis or periodontitis.”
The preferred method for interdental cleaning is the use of interdental brushes, with flossing restricted to situations where the gaps between teeth are too tight for a brush to enter without causing trauma.
Chemical agents, in mouth rinses and in toothpastes, used alongside mechanical plaque removal had “very clear and significant beneficial effects” in reducing gingival inflammation, explained Chapple. But he cautioned against patient self-medication because of possible side-effects and interactions with other substances in, for example, toothpastes. “They should only use these agents if advised to do so by oral health professionals”, he said.
Prof Chapple pointed out that there was no evidence to support the topical use of anti-inflammatory medication to control gingivitis and that the evidence for benefit following their systemic use was “incredibly thin”.
Prof Jepsen, chairman of the working group on primary prevention of peri-implant diseases, pointed out that half of patients with implants have peri-implant mucositits and 20 per cent develop peri-implantitis.
He outlined the importance of identifying bleeding around implants and crowns as a symptom of peri-implant mucositis, which needs to be successfully treated before it evolves into peri-implantitis. He emphasised that smoking was a big risk factor in peri-implantitis along with poor oral hygiene.
“The patient has to be instructed in proper oral hygiene measures and then it is possible to reduce the signs of inflammation quite significantly,” said Jepsen. “In addition, the professional has to do some plaque removal on a regular basis. And by doing so we are able to actually treat the mucositis.”
Secondary prevention, the process that begins once successful periodontal therapy has been applied to patients, represents a “weak link” in professional periodontal care, according to Prof Sanz, who chaired the working group on managing complications of gingival and periodontal diseases and professional mechanical plaque control. He stressed the need for good motivational techniques to keep patients visiting professionals.
Sanz said that studies show that more than 50% of patients stop visiting their dentist, although the secondary prevention of periodontitis is a “life-long” commitment.
Secondary prevention starts when treatment of periodontitis ends and Sanz stressed that “it is important to define our end-point of therapy.” He said that the Prevention Workshop agreed two targets – less than 15 per cent bleeding on probing and the elimination of pockets of 5mm or deeper – and “we need to treat until our patient is below these thresholds. That is when [secondary] prevention starts.”
Prof Tonetti added: “We have to recognise that the complete elimination of pockets may not be an attainable goal for all patient groups.”
Dentine sensitivity and halitosis (bad breath) were other topics covered in the 70-minute seminar, which concluded with a summary of the key messages of the Prevention Workshop.
Tonetti described the release of the workshop’s guidelines as a “time for renewed energy” in the prevention of periodontitis.
The proceedings and conclusions of the XI European Workshop in Periodontology, which was supported by educational grants from Procter & Gamble and Johnson & Johnson, are available online in a free, open-access supplement of the April 2015 issue of theJournal of Clinical Periodontology.




