Treatment, Article
How the modified free gingival graft can improve root-coverage results
15 December 2022

The free gingival graft is a tried-and-trusted technique used by periodontists in daily practice. However, the amount of root coverage gained when using this technique varies considerably. Olivier Carcuac, an EFP alumnus of the University of Gothenburg in Sweden, has modified the technique to improve its predictability. He explains the approach and its benefits.
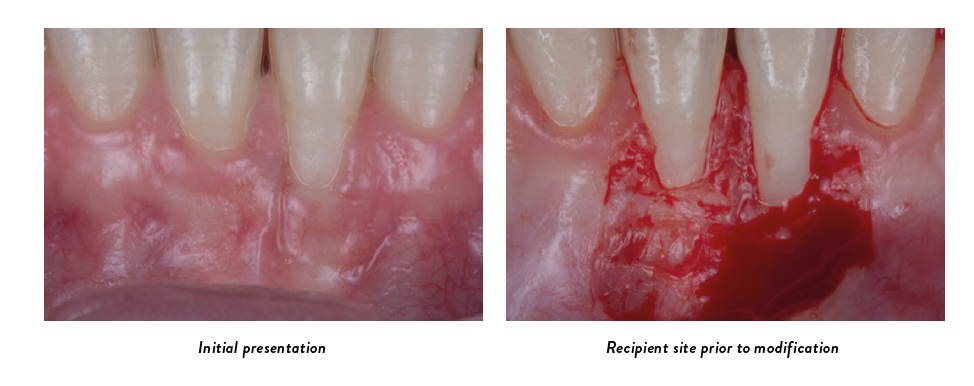
The free gingival graft (FGG) is commonly used for addressing gingival recession defects at lower incisors. However, from a clinical perspective, I noticed a great variability in terms of subsequent root coverage, a fact that has been reported in the literature (where root coverage ranges from 11% to 87%, with a mean of 72%). This poor predictability of root coverage when applying FGG has always been an issue for me.
When I tried to analyse the factors that might be implicated in such variable outcomes, I concluded that one of the technique’s inherent challenges is the limited blood supply to the FGG, because that part of the graft is positioned on an avascular recipient site (i.e., the exposed root surface). Limited blood supply to a graft means tissue necrosis, which I could clearly see in many cases of FGG in the marginal midfacial aspect of the recession defects.
I tried to find a way to address this limitation. My first attempts involved using biologics, such as enamel matrix derivative (EMD), to enhance the healing of the FGG in this critical area. Unfortunately,
these attempts were not conclusive. As a next step, I investigated whether it would be possible to prepare the recipient site differently.
The idea of modified free gingival graft (ModFGG) came about when I realised that every time I used FGG to increase the amount of keratinised tissue in an edentulous area, the outcome was always 100% successful — for the simple reason that the FGG could survive and integrate entirely because the recipient site was completely vascular. It then became obvious for me to apply this when using FGG to treat gingival recession defects at lower anterior teeth, and to develop a way of transforming the recipient site from a mixed vascular/avascular bed to a 100% vascular bed. This is what inspired me to develop the ModFGG concept.
ModFGG, step by step
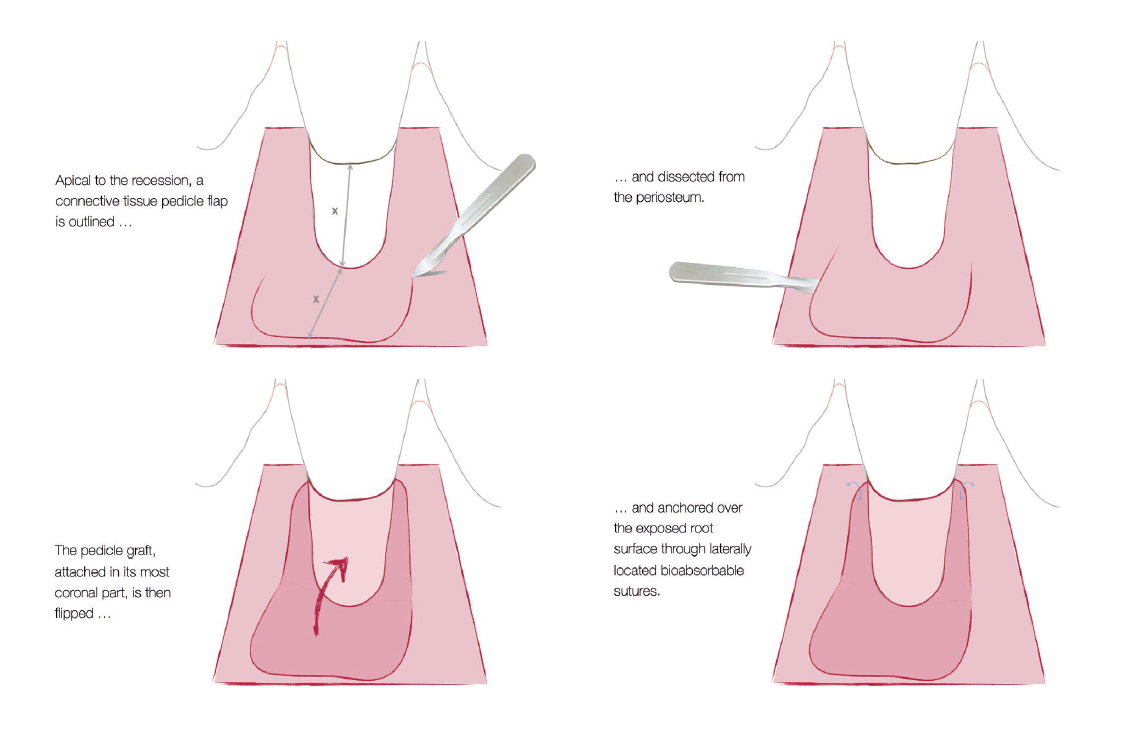
The ModFGG technique consists of a modification of the way the recipient site for conventional FGG is prepared. It involves four steps.

Preparation of the recipient site
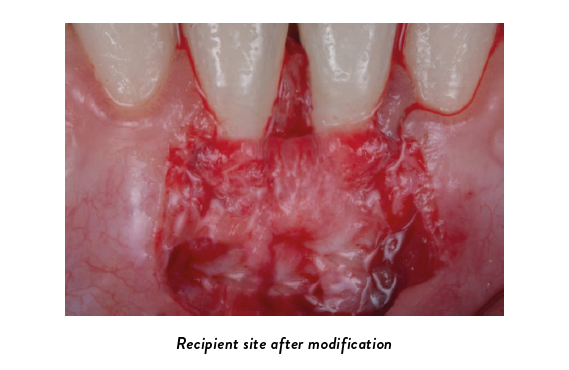
Following an intrasulcular incision, 2mm-long horizontal incisions at the level of the cementoenamel junction (CEJ) are performed bilaterally. From these, vertical releasing incisions are placed in a diverging manner, extending well into the alveolar mucosa. To prepare the recipient area, a thin partial-thickness flap is subsequently raised and then excised. The dimension of the resulting site is measured to obtain a foil template.

Apically to the exposed root area of the target teeth, a horizontal incision is placed at a distance corresponding to the height of the exposed root surface. From the endpoints of this incision, and running in a coronal direction, two slightly diverging incisions are added. The connective-tissue pedicle flap is thereby outlined, and it is then carefully dissected from the periosteum. The pedicle graft, attached in its most coronal part, is then flipped and anchored over the exposed root surface through laterally located bioabsorbable sutures.

Harvesting of the free gingival graft
Using the foil template, graft dimensions are outlined in the palate adjacent to the premolars and first molar. A partial-thickness graft consisting of epithelium and a thin layer of underlying connective tissue is harvested (with an intended total thickness of 1.5mm), maintaining a distance of ≥2mm to the maxillary teeth. Following harvesting of the FGG, several drops of high-viscosity cyanoacrylate tissue adhesive are applied to the palatal wound prior to coverage with a porcine-derived collagen sponge. The sponge is then stabilised by crossed sutures (6-0 non-resorbable monofilament).
"The poor predictability of root coverage when
applying FGG has always been an issue for me"
Placement of the graft
The FGG is adapted to the recipient site and anchored to the periosteum by means of simple interrupted sutures (6-0 non-resorbable monofilament). Suturing is continued along the lateral borders of the graft for complete stability. Vertically suspended crossed sutures are placed, when needed, to achieve a slight compression of the graft to the recipient site.
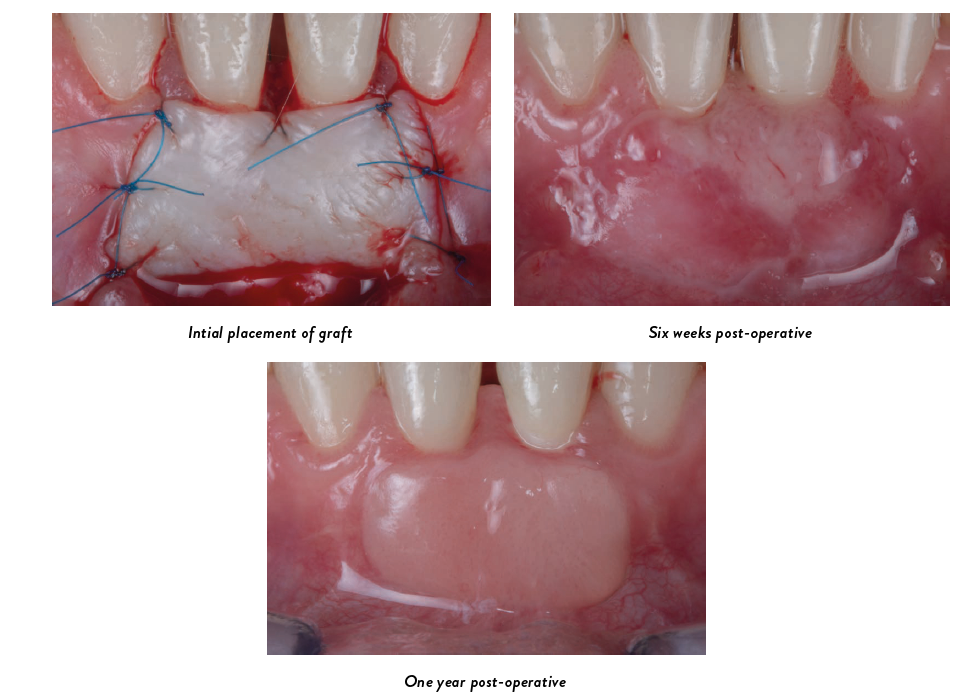
First trials
I did my first cases of ModFGG in 2019. My approach was to create a connective pedicle flap apical to the gingival recession defect and flip it coronally to cover the exposed root surface before positioning the FGG. I could apply this approach both at single and multiple recession defects at lower incisors, with the same successful outcomes.
In 2021, with Professor Jan Derks, I published a case series as a proof of concept (Oliver Carcuac, Jan Derks. “Modified Free Gingival Graft Technique for Root Coverage at Mandibular Incisors: A Case Series.” Int J Periodontics Restorative Dent, 2021 Mar-Apr; 41 (2): e37-e44. DOI: 10.11607/prd.5398).
Since 2019, I have applied the ModFGG concept in more than 100 patients with outcomes in terms of predictability and root coverage which are very similar to the ones we can achieve when using the connective tissue graft and the coronally advanced flap (CTG+CAF) at upper teeth.
Proving the concept and tips on use
From a scientific perspective, data from trials comparing ModFGG to conventional FGG and assessing the long-term efficacy of this novel technique were needed. Therefore, we recently completed a randomised controlled trial with a one-year follow-up comparing FGG and ModFGG. Single and multiple RT1 recession defects at lower incisors were included in this trial. The manuscript is now under peer review ahead of publication in a high-ranked journal.
Considering the results from our RCT, the ModFGG technique represents a valid approach for the management of single and multiple RT1 recession defects at mandibular incisors. The technique is superior to traditional FGG in terms of root coverage, gain and stability of keratinized tissue height, and patient satisfaction. I do not see any reason to continue using the conventional FGG approach, which is in my opinion outdated.
It is important to emphasise that I am still using other mucogingival surgical approaches — such as the vertically coronally advanced flap, the laterally closed tunnel, the laterally stretched flap, the coronally advanced tunnel, and vestibular incision subperiosteal tunnel access (VISTA) — for treating gingival recession defects at lower incisors. My decision on which technique to use depends on the clinical condition. But I am using the ModFGG approach whenever these other techniques cannot be applied, as in cases with short vestibule, highly attached frenum, complete lack of apical or lateral keratinised tissue, root prominence, or scar tissues.
Gingival-recession defects at lower incisors are probably the most difficult soft-tissue deficiencies around teeth to treat and require experienced clinicians. When applying the ModFGG, one critical aspect is the preparation of the apical connective-tissue pedicle. One of my recommendations to colleagues would be to make sure when preparing the recipient site (step 1) to remove only a very thin partial-thickness flap, to preserve enough connective-tissue thickness for the harvesting of the apical pedicle. I would really recommend to colleagues interested in applying the ModFGG in their everyday practice to attend hands-on workshops whenever possible to become familiar with the different steps of the technique and to start progressively with simple cases.
This article was original published in Perio Life: The EFP Alumni magazine, issue 4, in December 2022.
The full issue can be accessed here