Disease, Clinical & Translational Research, Article
Influence of systemic sclerosis on periodontal health
24 June 2024
The EFP recently awarded its Graduate Research Prize 2023 which promotes original graduate research. In the first of a series of articles by the four winners, Marianna Gavriiloglou (Université de Strasbourg, France) outlines a case-control study about how systemic sclerosis may influence periodontal health.
Systemic sclerosis or scleroderma (SSc) derives from the Greek words sclero (hard) and derma (skin) and involves the hardening of the skin. It is a rare chronic autoimmune disease characterised by tissue fibrosis, vasculopathy, and immune dysfunction. Patients with SSc present a progressive fibrosis of the skin and/or other organs.
Specifically, the localised cutaneous form of the disease (lcSSc) is defined when skin fibrosis is restricted to the face, neck, and area distal to elbows and knees, while the diffused cutaneous form (dcSSc) also includes skin fibrosis of the proximal limbs and/or trunk. Furthermore, various oral manifestations – both clinical and radiological – have been associated with the disease, such as microstomia, xerostomia, periodontitis, and the radiographic widening of the periodontal ligament (PDL) surface.
Unfortunately, treatments are not able to reverse the pathological effects of the disease. As a result, when disease is severe, dental treatments are challenging and often it has not been possible to treat patients appropriately. Therefore, the prevention and early management of oral diseases are of tremendous importance for this specific population.
The aim of this study was to compare the PDL surface of SSc patients with healthy controls using cone-beam computed tomography and to assess oral status, oral-health-related quality of life (OHRQoL), and gingival crevicular fluid (GCF) levels of different biomarkers between the two groups.
The study included 39 SSc patients and 39 matched healthy controls. Eighteen of the 39 SSc patients were diagnosed with the diffused form of the disease (dcSSc).
The main findings of this study include an increase of the PDL surface in SSc patients, which may be correlated with fibrosis and increased collagen deposition. It is worth mentioning that PDL thickening involves the whole root, without affecting tooth prognosis. Similar studies suggested that more than 30% of SSc patients present PDL widening at their radiographic examination.
A common clinical feature is the reduction of the mouth opening. In our study, only the dcSSc group had a statistically significant decrease of mouth opening, which highlights the proportional relationship between disease severity and the extent of fibrosis. Worsened oral health was confirmed, as SSc patients had a higher number of missing teeth and a higher decayed, missing, and filled Teeth (DMFT) index, as well as an increased gingival bleeding and attachment loss.
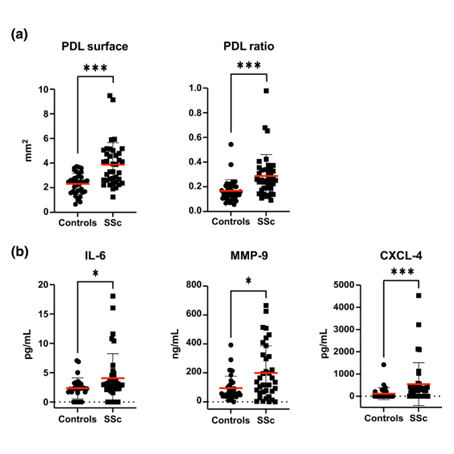
(a) PDL surfaces were measured (in square millimetre) on cone‐beam computed tomography (CBCT) axial sections. The PDL ratio represents the normalization of the PDL surface on the root surface. (b) Concentrations of interleukin‐6 (IL‐6; in picograms per millilitre), matrix metalloproteinase 9 (MMP‐9; in nanograms per millilitre) and chemokine (C‐X‐C motif) ligand 4 (CXCL‐4; in picograms per millilitre) were measured by enzyme‐linked immunosorbent assay in the GCF of SSc patients (black circles) and controls (black squares). The red bars represent the mean concentrations and the black bars standard deviations. Significant results of the Wilcoxon signed ranked test are indicated are indicated (*p < .05; ***p < .001).
Interestingly, gingival bleeding was less in dcSSc group compared to lcSSc group, probably because of extensive fibrosis, which masks signs of inflammation. According to Pischon et al. (2016), SSc patients present a distinct pattern of periodontitis, which includes increased periodontal attachment loss and decreased gingival bleeding. It has been shown that microvascular alterations may affect periodontal vascularisation, having negative effects on immune response and tissue healing capacities.
In addition, elevated levels of biomarkers (interleukin-6, matrix metalloproteinase-9, and chemokine ligand-4) were found in the GCF of SSc patients, indicating increased inflammation, tissue degradation, and a potential early prediction of severe complications. Furthermore, the scores of OHRQoL were significantly impaired in SSc patients and especially in those with dcSSc, which underlines the influence of tissue fibrosis on OHRQoL. In a multivariable analysis, OHRQoL score, higher number of missing teeth, and lower mouth opening were significantly correlated with the dcSSc group. Nevertheless, no correlation was found between periodontal parameters and disease features in either univariate or multivariate analysis.
To conclude, PDL surface widening could be a hallmark of SSc severity. This study also highlights that oral complications of SSc patients are an existing reality, even though they are often overshadowed. SSc patients should have a regular monitoring of their oral health and a targeted dental care. It is important to promote preventive care programmes and a closer communication between medical experts for the treatment of these specific patients.
▪ This article is based on: Sophie Jung, Marianna Gavriiloglou, François Séverac, Lucille Haumesser, Amira Sayeh, Emmanuel Chatelus, Thierry Martin, Olivier Huck, (2023). ‘Influence of systemic sclerosis on periodontal health: A case-control study’. Journal of Clinical Periodontology 50(10), 1348-1359. doi: 10.1111/jcpe.13846
Note: The EFP Graduate Research Prize seeks to promote original graduate research, performed within the framework of postgraduate training the federation’s accredited graduate programmes in periodontology. It is awarded annually in two categories: clinical research and preclinical/basic research. It is open to all students of EFP accredited graduate programmes in periodontology.
Bibliography
Baron, M., Hudson, M., Tatibouet, S., Steele, R., Lo, E., Gravel, S., … Gornitsky, M. (2014). The Canadian systemic sclerosis oral health study: Orofacial manifestations and oral health-related quality of life in systemic sclerosis compared with the general population. Rheumatology (Oxford, England), 53(8), 1386‑1394. doi: 10.1093/rheumatology/ket441
Baron, M., Hudson, M., Dagenais, M., Macdonald, D., Gyger, G., El Sayegh, T., … Gornitsky, M. (2016). Relationship Between Disease Characteristics and Oral Radiologic Findings in Systemic Sclerosis: Results From a Canadian Oral Health Study. Arthritis Care & Research, 68(5), 673‑680. doi: 10.1002/acr.22739
Cutolo, M., Soldano, S., & Smith, V. (2019). Pathophysiology of systemic sclerosis: Current understanding and new insights. Expert Review of Clinical Immunology, 15(7), 753–764. https://doi.org/10.1080/1744666X.2019.1614915
Dagenais, M., MacDonald, D., Baron, M., Hudson, M., Tatibouet, S., Steele, R., … Gornitsky, M. (2015). The Canadian Systemic Sclerosis Oral Health Study IV: Oral radiographic manifestations in systemic sclerosis compared with the general population. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 120(2), 104‑111. doi: 10.1016/j.oooo.2015.03.002
Iordache, C., Antohe, M.-E., Chirieac, R., Țănculescu, O., Ancuța, Ancuța, E., & Ancuța, C. (2019). Volumetric Cone Beam Computed Tomography for the Assessment of Oral Manifestations in Systemic Sclerosis: Data from an EUSTAR Cohort. Journal of Clinical Medicine, 8(10), 1620. doi: 10.3390/jcm8101620
Jung, S., Martin, T., Schmittbuhl, M., & Huck, O. (2017). The spectrum of orofacial manifestations in systemic sclerosis: A challenging management. Oral Diseases, 23(4), 424–439. https://doi.org/10.1111/odi.12507
LeRoy, E. C., Black, C., Fleischmajer, R., Jablonska, S., Krieg, T., Medsger, T. A., Jr., Rowell, N., & Wollheim, F. (1988). Scleroderma (systemic sclerosis): Classification, subsets and pathogenesis. The Journal of Rheumatology, 15(2), 202–205
Pischon, N., Hoedke, D., Kurth, S., Lee, P., Dommisch, H., Steinbrecher, A., … Riemekasten, G. (2016). Increased Periodontal Attachment Loss in Systemic Sclerosis Patients. Journal of Periodontology, 1‑12. doi: 10.1902/jop.2016.150475
Scardina, G. A., Pizzigatti, M. E., & Messina, P. (2005). Periodontal microcirculatory abnormalities in patients with systemic sclerosis. Journal of Periodontology, 76(11), 1991‑1995. doi: 10.1902/jop.2005.76.11.1991

Biography
Marianna Gavriiloglou is a current PhD student in the department of periodontology at the Aristotle University of Thessaloniki in Greece, where she received her degree in dentistry in 2019. In 2023, she completed her postgraduate studies in periodontology and implantology at the University of Strasbourg, France under the guidance of Prof. Olivier Huck. She also works as a specialist in periodontology and implants in a dental office in Greece. She is a member of the Hellenic Society of Periodontology and Implant Dentistry.




