
Issue No. 128
Summarised from Journal of Clinical Periodontology, Volume 51, Issue 8, August 2024, 997-1004
Editor: Andreas Stavropoulos, chair, EFP scientific affairs committee
Can we avoid surgery for peri-implantitis with systemic antibiotics?
Authors: Jarno Hakkers, Tine E. Vangsted, Arie Jan van Winkelhoff, Yvonne C. M. de Waal
Background
Treating peri-implantitis, an inflammatory condition affecting the tissues around dental implants, has many complexities and challenges. As this disease affects the soft and hard tissues, management strategies – including non-surgical and surgical interventions – aim to reduce inflammation, decrease probing pocket depth, and end bone loss around implants. While non-surgical sub-marginal instrumentation (NSI) can lead to improvements in clinical parameters such as bleeding scores, residual or recurrent inflammation is still common post-treatment. As a result, researchers often explore additional therapies to enhance the outcomes of non-surgical peri-implantitis treatment. One such approach under investigation is the use of systemic antimicrobials as adjuncts to non-surgical treatment. When NSI fails to achieve peri-implant health, the use of antimicrobials might prove useful in avoiding surgery. In progressive peri-implantitis (pockets over 7mm and severe suppuration), antibiotic therapy might spare the need for peri-implantitis surgery. This study seeks to contribute to the enhancement of clinical practices by shedding light on the potential role of systemic antibiotics in influencing the need for surgical interventions following non-surgical treatment of peri-implantitis, thereby advancing the understanding and management of this complex dental issue.
Aim
To assess the prolonged impacts of systemically administered amoxicillin and metronidazole, alongside non-surgical sub-marginal instrumentation, and to evaluate the requirement for additional surgical treatment during the aftercare programme.
Materials & methods
- The study was designed as a retrospective cohort following patients for an average of 36 months after their participation in a previous three-month randomised controlled trial (RCT).
- Patients were randomly assigned to receive non-surgical submarginal instrumentation (NSI), with additional systemic antibiotics – systemic amoxicillin and metronidazole, 500/500mg, three times daily for seven days – (group AB+), or not (group AB-).
- NSI consisted of multiple sessions of mechanical cleaning performed by proficient dental hygienists. This process involved supra- and submucosal cleansing of implants and teeth using an air polisher equipped with a sub-gingival tip, along with ultrasonic instruments.
- The need for additional surgical treatment was assessed based on pocket depth (PD) >5mm and concomitant bleeding and/or suppuration on probing.
- Clinical and radiographic data was collected at T0 (pre-NSI), T1 (three months post-NSI), and T2 (the last available follow-up visit).
- The primary outcome of the study was to evaluate the need for additional surgical therapy post-NSI.
- Secondary outcomes included monitoring changes in peri-implant and periodontal probing depths (PD), bleeding and suppuration scores (BS, SS), and plaque scores (PS). Clinical treatment success at T2 was evaluated according to predetermined criteria.
Results
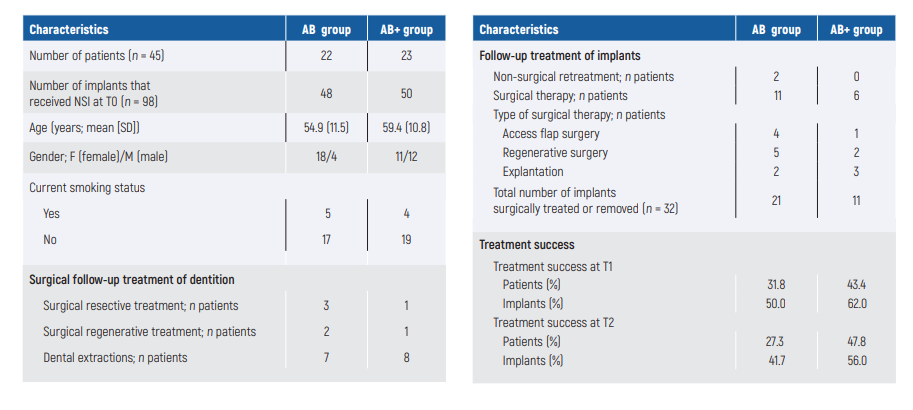
- Initially, 57 patients participated in the study. However, 12 of them did not participate in the aftercare programme, resulting in a final cohort of 45 patients (23 in the AB+ group and 22 in the AB- group) included in the final analysis. The average follow-up duration was 35.9 months, ranging from six to 80 months.
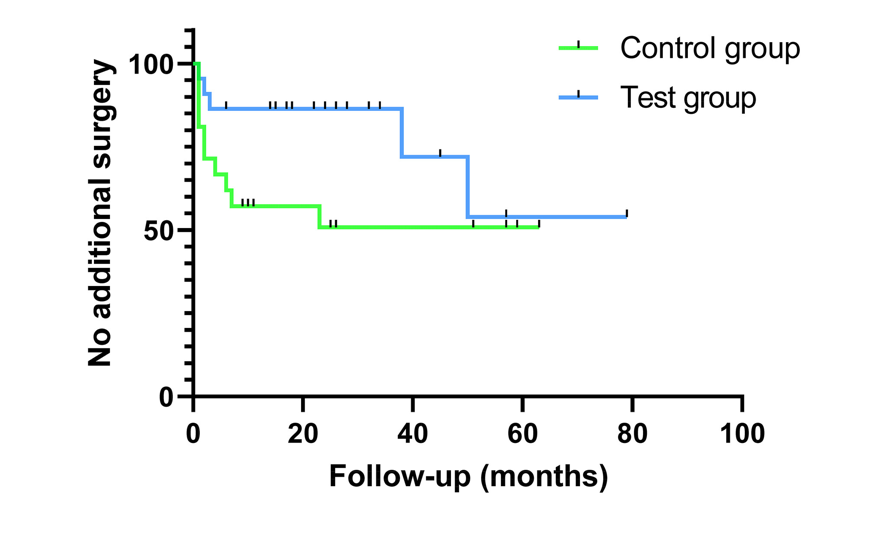
- A total of 62.2% of patients did not require additional periimplantitis surgery. Variations were observed between the AB+ group (73.9%) and the AB- group (50.0%) over a 36-month duration. However, the overall results did not reach statistical significance.
- A difference in the number of surgeries recommended within the initial 36 months was observed. Specifically, in the AB+ group, there was an increase in surgeries observed after this timeframe, suggesting a potential effective period of approximately three years where antibiotics, as part of a robust postoperative care protocol, may have had an impact on patient outcomes. However, the overall results did not reach statistical significance.
- The study revealed that the covariates did not show time dependency (p>.05) and adjusting for these factors did not significantly alter the hazard ratio for future surgery related to antibiotic use.
- Both groups initially improved peri-implantitis parameters significantly, with variations between both groups over time. The AB- group showed a continued significant reduction from T1 to T2. Significant reductions in SS and PS were observed between T0 and T1, with a significant decrease in PS specifically noted in the AB- group from T1 to T2. Both groups exhibited a slight increase in PS at T2.
Limitations
- The retrospective nature of the study necessitates careful interpretation because of inconsistencies in data-storage practices with patient files.
- The customised aftercare programme resulted in diverse follow-up intervals and durations, impacting the study's consistency.
- Treatment success relied solely on clinical parameters because of the absence of radiographic records, which limits assessment of peri-implant bone loss during the follow-up.
- No data was provided concerning the keratinised gingiva around the implants.
- Regarding the treatment method, only the exposed implant areas were cleaned, and how the groove areas were cleaned subgingivally was not addressed.
- The study's sample size was relatively small, potentially impacting the generalisability of findings.
- There was no data on the types of implants and specifically their surface characteristics.
Conclusions & impact
- Using amoxicillin and metronidazole alongside non-surgical implant treatment (NSI) does not prevent the need for additional surgical treatment for peri-implantitis in the long term. However, there is a positive effect within the first three years following NSI, especially when combined with supportive peri-implant care.
- Initial PDs could influence the outcome following nonsurgical treatment alone.
- Some patients will benefit from adjunctive antibiotics when combined with non-surgical treatment, yet it will not prevent the need for surgery.
Rapporteurs: Nora Jaber, Noa Frank, David Domb, and Adi Schwartz, supervised by Asaf Wilensky
Affiliation: Postgraduate programme in periodontology at Hadassah-Hebrew University Medical Center, Jerusalem, Israel
With kind permission from Wiley Online Library. Copyright © 1999-2024 John Wiley & Sons, Inc. All rights reserved




