
Issue No. 130
Summarised from Journal of Clinical Periodontology, Volume 51, Issue 10, October 2024, 1277-1288
Editor: Andreas Stavropoulos, chair, EFP scientific affairs committee
Non-surgical retreatment or papillary preservation flap surgery?
Authors: Luigi Barbato, Desirée Noce, Maria Di Martino, Walter Castelluzzo, Folco Spoleti, Cosimo Rupe, Michele Nieri, Francesco Cairo
Background
The main goal of periodontal treatment is arresting disease progression by reducing bleeding on probing (BoP), probing pocket depth (PPD), and clinical attachment loss. Non-surgical treatment of periodontitis (steps 1 and 2) is largely effective in terms of reducing BoP and PPD reduction and increasing the clinical attachment level (CAL).
However, treatment outcomes can be influenced by smoking, oral-hygiene habits, and tooth-related factors. Several studies demonstrated that, after initial treatment, PPD ≤4mm without BoP is associated with more stable periodontal status, while PPD ≥6mm and BoP ≥30% are considered risk factors for future tooth loss.
When cause-related therapy is completed and bleeding pockets with PPD >4mm or deep pockets with PPD >5mm remain, step 3 of periodontal therapy is indicated (i.e., repeated subgingival instrumentation, access flap/resective or regenerative periodontal surgeries). Non-surgical treatment is recommended for moderate pockets with shallow intraosseous defects, while periodontal regenerative surgery is recommended for deep residual pockets harbouring intraosseous defects ≥ 3mm.
The efficacy of non-surgical reinstrumentation (NSR) compared with surgery is controversial. Classic studies support flap surgery for better PPD reduction and clinical attachment gain in deep pockets, compared to scaling and root planing. However, recent techniques—such as minimally invasive non-surgical technique (MINST)—have shown good clinical outcomes.
Aims
This randomised controlled trial compared the efficacy of non-surgical reinstrumentation (NSR) and papillary preservation flap (PPF) surgery at single-rooted teeth with residual pockets.
Materials & methods
- Study design: parallel, single-center, blinded examiner, randomised clinical trial.
- Patient cohort: 46 patients (≥18 years) with periodontitis.
- Interventions:
- Oral-hygiene instructions and non-surgical periodontal therapy (steps 1 and 2) with a minimally invasive non-surgical technique (MINST).
- Re-evaluation 12–14 weeks after initial therapy: patients with at least one residual pocket with PPD ≥5 mm were randomly assigned to either subgingival debridement following MINST principles (control) or PPF (test).
- In the case of more than one site meeting the inclusion criteria, the deepest one was considered as the experimental one.
- Clinical measurements: PPD, gingival recession (Rec), CAL, BoP, plaque index (PI), keratinized tissue (KT), tooth mobility, full-mouth plaque score (FMPS), full-mouth bleeding score (FMBS), distance (mm) from the tip of the papilla and the contact point of mesial and distal to the experimental tooth and mucogingival junction (CP–TP) measured at the middle buccal point.
- Clinical measures were registered at baseline, three and six months after therapy
- Periapical x-rays were taken at baseline and after six months and the distance (in mm) between the bone crest (BC) and the bottom of the defect (BC–DB) was assessed.
- Outcome measures:
- PPD reduction at the six-month follow-up.
- CAL gain, pocket closure (i.e., PD ≤4 mm and absence of BoP), chair time, patient-reported outcome measures (PROMs), overall satisfaction, aesthetic satisfaction.
- Statistical analysis: Analysis of Covariance (ANCOVA), Fisher's Exact Test, Student's t-tests.
Results
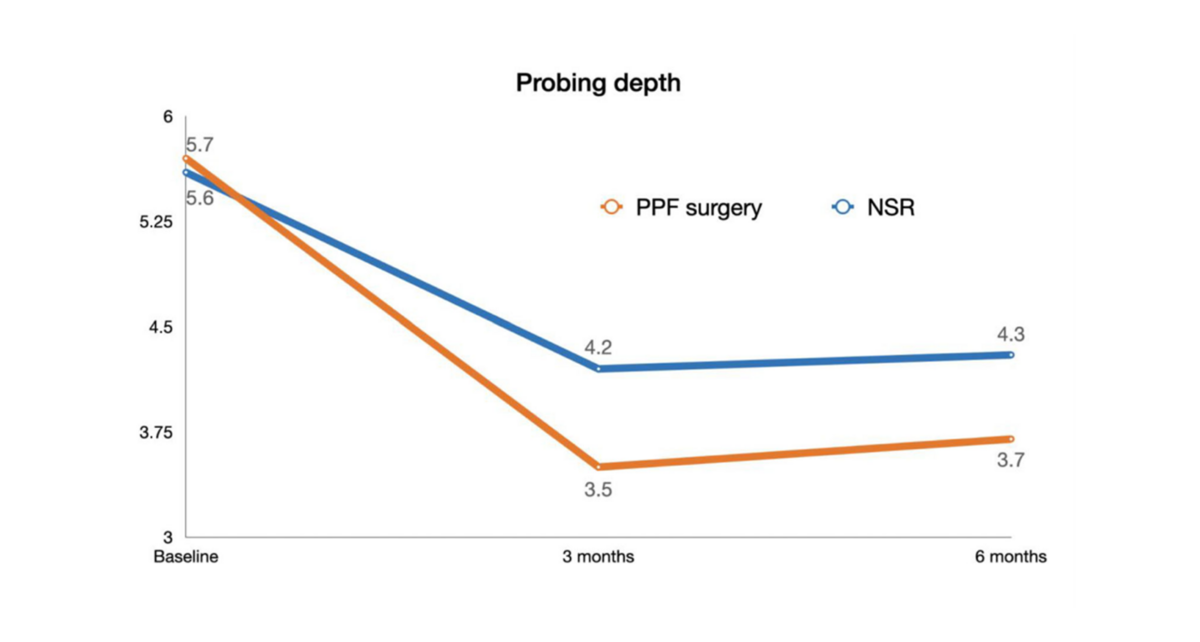
- At six months, both treatments resulted in significant PPD reduction, 2.0 ± 0.7mm (p < 0.001) in PPF group and 1.3 ± 1.0mm (p =0.009) in NSR group, without statistically significant difference (p = 0.167).
- CAL gain was 1.4 ± 0.8mm (p < 0.001) in PPF group and 1.0 ± 2.4 mm (p = 0.071) in NSR group (p = 0.368).
- Pocket closure was higher in the PPF group (86%) than in the NSR group (61%) (p = 0.091).
- Recession increased by 0.3 ± 0.6mm (p = 0.031) in the NSR group and by 0.6 ± 0.5mm (p < 0.001) in the PPF group.
- The differences between groups in terms of recession (p = 0.073) and keratinized tissue changes (p = 0.504) were not significant.
- More NSR-treated sites were BoP+ (61% vs. 27%; p = 0.036).
- BC–BD was reduced by 0.3 ± 0.5mm in the PPF group and 0.1 ± 0.9mm in the NSR group.
- Smoking was associated with less PPD reduction (p = 0.036) and CAL gain (p = 0.053) in both groups.
- Treatment time was longer for the PPF group with a mean duration of 20.5 ± 7.1 minutes compared to 6.9 ± 1.5 minutes for the NSR group.
- One patient in the NSR group developed a periodontal abscess at six months.
- PROMs and post-operative pain were similar in both groups.
Limitations
- Inclusion of only single-rooted teeth with shallow infrabony defects may impact the ability to generalize from the conclusions.
- The higher PPD reduction at three months for PPF compared to NSR was not maintained at six months, suggesting that the benefit of surgery may decrease over time. Initial improvements may not translate into long-term clinical significance.
- A difference of 0.5mm between treatments was considered to determine statistical significance which may be questioned from a clinical point of view.
- Larger multi-center studies are needed to validate these findings.
Conclusions & impact
- This study is the first randomised clinical trial to compare the clinical efficacy of non-surgical and surgical treatments in treating residual periodontal pockets at single-rooted teeth.
- NSR and PPF surgery are two effective procedures accepted by patients which reduce probing depth at six months, without significant difference between the groups.
- Controlling risk factors such as smoking is a key point in both treatments to improve clinical outcomes.
- Pocket closure may be less predictable with NSR: five out of 23 sites showed no PPD improvement and one patient developed a periodontal abscess requiring additional surgery.
- In the therapeutic decision between surgical and non-surgical treatments, it is important to take into consideration the number of residual pockets at the involved teeth, the general needs of the patient, and the additional costs of the surgeries.
Rapporteurs: Amélie Sarbacher, Lina Tahour, Simone Sbalchiero, Aikaterini Vasileiou, and Eirini Militsi, supervised by Prof. Olivier Huck
Affiliation: Postgraduate programme in periodontology, University of Strasbourg, Strasbourg, France
With kind permission from Wiley Online Library. Copyright © 1999-2024 John Wiley & Sons, Inc. All rights reserved




