
Issue No. 127
Summarised from Journal of Clinical Periodontology, Volume 51, Issue 7, July 2024, 936-965
Editor: Andreas Stavropoulos, chair, EFP scientific affairs committee
Short versus long implants: when does size matter?
Authors: Andrea Ravidà, Matteo Serroni, Wenche S. Borgnakke, Mario Romandini, I-Ching (Izzie) Wang, Claudia Arena, Marco Annunziata, Gennaro Cecoro, Muhammad H. A. Saleh
Background
Post-extraction horizontal and vertical ridge dimensional changes may affect the complexity of implant treatment. Augmentation procedures, such as maxillary sinus elevation and mandibular supracrestal bone augmentation, are available to mitigate the anatomical challenges of ridge resorption. But they often require high technical skills from clinicians, increase the costs and duration of treatment, and carry higher risks of complications and patient morbidity. Therefore, the use of short dental implants (≤6mm) in atrophic posterior sites has been proposed as an alternative treatment option. However, the evidence supporting the use of short implants is not robust. Previous systematic reviews have not separately examined short and long implants in different clinical scenarios, while factors such as bone quality, location in the mouth, and the type of edentulism being reconstructed have not been considered, although they may affect the success of short implants.
Aim
To evaluate the survival rates (primary outcome), as well as marginal bone loss (MBL) and complications of short implants (≤6mm) compared to long implants (≥10mm) in specific clinical scenarios.
Materials & methods
- A systematic review/meta-analysis of randomised controlled trials (RCTs), with no restrictions in terms of publication date or language, was conducted to evaluate implant survival, MBL, and biological and prosthetic complications in short (≤6mm) implants compared to long (≥10mm) implants.
- Studies examining patients of any age, comparing ≥1 short (≤6mm) with ≥1 standard-length (≥10mm) dental implants (with or without bone augmentation), restored with a fixed prosthesis and a one-year follow-up were included.
- The systematic review followed the Cochrane Handbook guidelines and results were reported according to the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
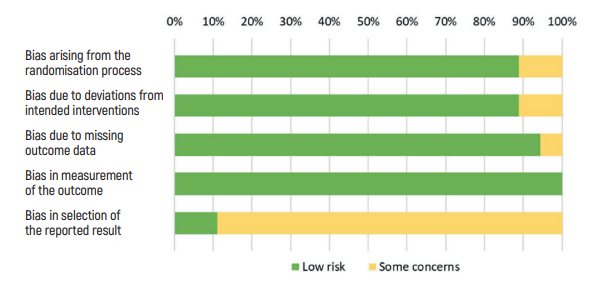
- Risk of bias was assessed through the Cochrane risk-of-bias tool.
- Meta-analyses were conducted upon stratification of ≥2 studies with the same exposure, outcome, and observation duration.
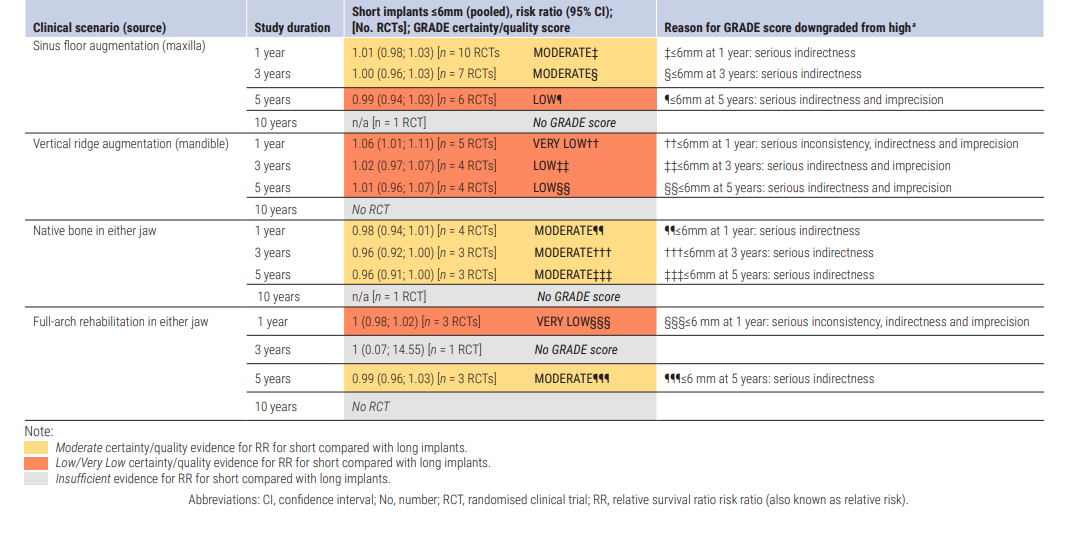
- Certainty or quality of evidence was evaluated according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach.
- A subgroup analysis by type of bone augmentation procedure in the control group (vertical bone augmentation in the mandible, sinus lift in the maxilla, none, native bone) and type of restoration (full-arch rehabilitations or others) was performed.
Results
- A total of 19 RCTs were included, which comprised a total of 1,097 short (≤6mm) and 1,117 long (≥10mm) implants.
- 10 RCTs compared the survival rate of ≤6mm implants versus ≥10mm implants placed after maxillary sinus lifting.
- There is high-certainty evidence that 6mm implants have similar survival and complication rates compared to ≥10mm implants placed after maxillary-sinus floor elevation.
- There is inconclusive evidence for shorter implants (4-5mm) as alternatives to long implants (≥10mm) placed after maxillary sinusfloor elevation.
- Five RCTs compared the survival rate of ≤6mm versus ≥10mm implants placed in native bone.
- There is moderate-certainty evidence that short implants (≤6mm) have similar survival and complication rates compared to long implants (≥10mm) when placed in native bone (either jaw).
- Three RCTs compared the survival rate of ≤6mm versus ≥10mm implants placed for full-arch rehabilitations.
- There is moderate-certainty evidence that short implants (≤6mm) have similar survival and complication rates compared to long implants (≥10mm) as part of a full-arch rehabilitation (either jaw).
- Six RCTs compared the survival rates of ≤6mm versus ≥10mm implants placed in vertically augmented mandibular bone.
- There is inconclusive evidence that short implants (≤6mm) have similar survival and complication rates compared to long implants (≥10mm) in vertically augmented mandibular bone.
- Two RCTs reported reduced costs and higher patient satisfaction with the use of 6mm implants compared to ≥10mm implants.
Limitations
- Non-RCT longitudinal intervention studies of high quality were not included in the study but might also have been of value to examine.
- Because of heterogeneity and insufficient number of studies, subgroup analysis to evaluate the following confounding factors was not possible:
- Implant factors – materials, widths, macro-design, surface characteristics.
- Surgical factors – technical approach, biomaterials, healing time.
- Population characteristics – age, ethnicity, sex.
- Site and placement factors – implant location, tilted or axially positioned. - Patient-reported outcome measures were not examined.
Conclusions & impact
The results support the use of 6mm implants as an alternative treatment option to sinus lifts with long implants (≥10mm), as well as the use of short implants (≤6mm) placed in native bone or as part of full-arch rehabilitations in either jaw. • The evidence backing the use of short implants (≤6mm) in vertically augmented mandibular ridges is inconclusive. • The lack of moderate- or high-certainty evidence to support other lengths or clinical scenarios does not imply that short implants should not be placed in these situations, but only that evidence from the examined RCTs is insufficient. • Future research should evaluate specific implant lengths individually instead of as a group (e.g., ≤6mm) and for specific clinical scenarios.
Rapporteurs: Jackie Yiu and An-Lun Cheng supervised by Dr Su Sheng Quach, Assoc. Prof. Ryan Lee, and Prof. Saso Ivanovski
Affiliation: Postgraduate programme in periodontology at the University of Queensland, Brisbane, Australia
With kind permission from Wiley Online Library. Copyright © 1999-2024 John Wiley & Sons, Inc. All rights reserved




