Issue No. 131
Summarised from Journal of Clinical Periodontology, Volume 51, Issue 11, November 2024, 1534-1544
Editor: Andreas Stavropoulos, chair, EFP scientific affairs committee
Soft-tissue augmentation at immediate implant placement: Why rush?
Authors: Jan Cosyn, Thibault Struys, Pieter-Jan Van Hove, Stefanie De Buyser, Thomas De Bruyckere
Background
Immediate implant placement (IIP) enables tooth replacement with minimal surgery, providing an instantaneous temporary prosthesis alongside an acceptably high implant survival rate. The stability of buccal soft tissue related to IIP is a concern because of the inevitable post-extraction bone remodelling/resorption. Grafting the gap between the implant and the buccal bone wall and soft-tissue augmentation (STA) are two approaches to counteract this undesirable phenomenon.
Clinical trials have documented the approach of combining STA and IIP. While combining these two procedures in a single surgery favours patients, it may make the surgical intervention challenging. Creating a pouch in thin buccal mucosa increases the risk of buccal perforation and disrupts the blood supply of the underlying buccal bone wall.
In contrast, performing STA three months after IIP allows clinicians to limit STA to those scenarios in which soft-tissue correction is necessary. It is also easier to create a pouch in the buccal mucosa when it has already thickened after healing from the extraction. Some degree of buccal bone remodelling occurs within the three months after extraction, but performing a buccal pouch surgery at that time may limit further buccal bone resorption. This clinical trial aims to evaluate this hypothesis.
Aims
This single-centre randomised controlled trial assessed the effect of soft-tissue augmentation (STA) timing on buccal bone changes at one year, when performed together with or three months after immediate implant placement (IIP).
Materials & methods
- Patients enrolled in the trial had one failing tooth in the anterior maxilla. The site had at least one neighbouring tooth, adequate apical or palatal alveolar bone for primary implant stability, and an intact buccal bone wall following tooth removal.
- Patients were premedicated (amoxicillin 2000 mg and ibuprofen 600 mg) one hour before surgery. After non-flap tooth removal, implants (Straumann BLX RB diameter 3.75 mm, Straumann) were placed using a surgical guide with a minimum stability of 25 N·cm.
- The implant shoulder was positioned 4 mm below the midfacial soft-tissue margin. The gap between the implant and the buccal bone wall was filled with C-DBBM (Bio-Oss Collagen, Geistlich Pharma AG) up to the level of the implant shoulder. Implant abutments were installed, and temporary screw-retained acrylic crowns were delivered within two days.
- Patients were randomly allocated to the control group, where soft-tissue augmentation was performed immediately after implant placement (ISTA), or to the test group, where the same intervention was delayed and performed after three months (DSTA).
- The connective tissue graft (CTG) was prepared in the proper dimensions from a free gingival graft taken from the palatal mucosa in the premolar area. It was brought into the prepared mucosal pouch and fixed to the buccal mucosa with two single sutures.
- Changes in the buccal-bone and soft-tissue dimensions were assessed through the superimposition of CBCT images taken before tooth extraction and one year after implant placement.
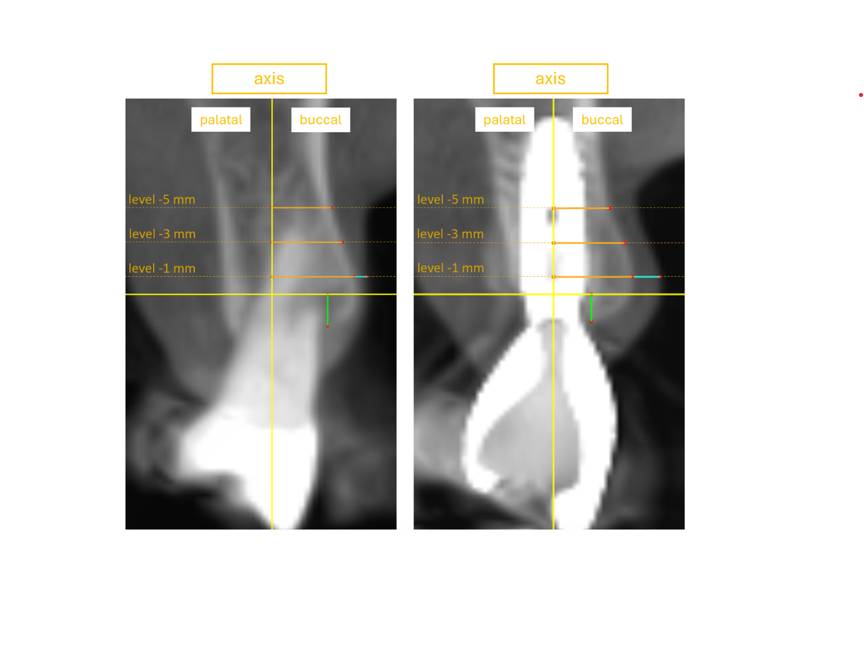
Vertical yellow line, reference line through the long axis of the implant; horizontal yellow line, reference line perpendicular to the long axis at the level of the implant-abutment interface. Dotted brown lines, horizontal measurement levels at −1, −3, and −5 mm from the implant-abutment interface. Brown full lines, horizontal buccal bone level at −1, −3, and −5 mm from the implant-abutment interface. Magenta line, buccal soft-tissue thickness. Green line, vertical buccal bone level.
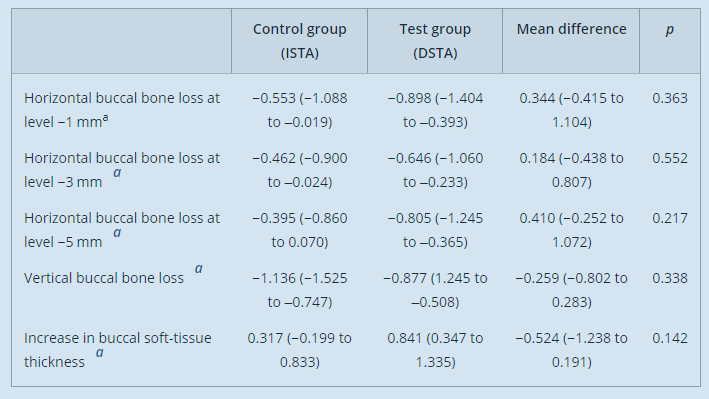
a = estimated marginal mean in millimetres (95% confidence interval).
Results
- A total of 20 patients were assigned to each group (control: 16 females and four males, average age 57.6; test: 9 females and 11 males, average age 54.2). Ten patients in the control group and 13 patients in the test group exhibited a thick-bone-wall phenotype. Most patients were periodontally healthy or had been treated for periodontitis stage I or II.
- At 1 mm below the implant shoulder, the estimated marginal mean horizontal buccal bone loss was −0.553 mm for the control group and −0.898 mm for the test group. The estimated mean difference of 0.344 mm favouring the control group was not significant. The horizontal buccal bone loss evaluated at a more apical level also favoured the control group, but without a significant difference compared to the test group.
- The estimated increase in buccal soft-tissue thickness was 0.317 mm for the control group and 0.841 mm for the test group. The mean difference of −0.524 mm, favouring the test group, was not significant.
- The study considered the regeneration – i.e., a combination of socket grafting and STA – to be successful when it can counteract any buccal soft-tissue loss at a level of -1 mm. Both groups showed no statistically significant difference in the percentage of successful regeneration (p=1.000), achieved in 82% of the patients in the control group and 75% in the test group.
Limitations
- The lack of balance between male and female participants in both the test and the control group may confound the results, as female individuals are associated with thin phenotypes.
- The study included sites with a thin buccal bone wall (<1 mm), where it has been demonstrated in several studies that buccal hard- and soft-tissue remodelling could be less predictable at those sites. This may contribute to the study's finding of non-significance.
- The dimensions of connective-tissue grafts were not controlled (or at least were impracticable to control) or measured. In addition, the healing time following the STA was not equal between the test (nine months) and the control (12 months). These factors may affect the soft-tissue dimension evaluated at one year.
Conclusions & impact
- In immediate implant placement (IIP) and socket grafting at anterior maxillary sites where the buccal bone wall is intact, the timing of soft-tissue augmentation (STA) does not appear to affect the extent of buccal bone loss.
- The hypothesis that buccal mucosa manoeuvres to create a pouch for the connective-tissue graft during IIP may disrupt the vascularisation between the mucosa and periosteum – and potentially compromise the buccal bone – is not supported by the results of this study.
- Clinicians and patients can choose a suitable time for STA, considering practical factors such as the reduction of surgical intervention, implant-abutment reconnection, or the difficulty of soft-tissue manipulation at IIP.
Rapporteurs: Chuachamsai Sompol, Federica Romano, Giacomo Baima, and Giulia Maria Mariani, supervised by Professor Mario Aimetti
Affiliation: Postgraduate programme in periodontology, C.I.R. Dental School, University of Turin, Turin, Italy.
With kind permission from Wiley Online Library. Copyright © 1999-2024 John Wiley & Sons, Inc. All rights reserved