
Issue No. 132
Summarised from Journal of Clinical Periodontology, Volume 51, Issue 12, December 2024, 1656-1664
Editor: Andreas Stavropoulos, chair, EFP scientific affairs committee
What are the 10-year outcomes of dental implants in narrow alveolar ridges?
Authors: M. Alami, N. Ntovas, G. Penne, W. Teughels, M. Quirynen, A. Castro, A. Temmerman
Background
In terms of bone resorption after dental extraction, the buccal plate tends to experience greater loss compared to the lingual/palatal plate, with horizontal dimensional changes being more prominent.
It is recommended that a minimum buccal bone thickness of 1–2mm should be maintained to safeguard the buccal plate and provide adequate soft-tissue support around dental implants. When the alveolar ridge dimensions are insufficient, bone-augmentation procedures are often needed to achieve successful implant-supported rehabilitation. However, these procedures require advanced surgical expertise and are linked to higher morbidity, extended treatment duration, and increased costs.
Avoiding augmentation procedures may help in minimizing post-operative complications, lowering treatment expenses, and facilitating patient recovery. Moreover, patients generally tend to favour minimally invasive approaches. Provided there is long-term dimensional stability of thin buccal plates, the need for augmentation may be superfluous, thereby simplifying the overall treatment process.
Aim
This study aimed to evaluate 10-year outcomes of implants placed in ridges with limited bucco-oral width (≤4.5mm) without bone augmentation. Radiological interproximal bone changes, cumulative survival rates, and clinical parameters were assessed to determine the long-term stability and success of this simplified treatment approach.
Materials and methods
This prospective case series was carried out at KU Leuven, Belgium, involving 28 patients who received a total of 100 implants between 2009 and 2010.
- Inclusion criteria for eligibility consisted of:
- Patients 18 years old or older.
- Implant sites with a bucco-oral width of ≤4.5mm, confirmed by using CBCT.
- Patients who prioritize function over aesthetics.
- Exclusion criteria were the absolute contraindications for implant therapy.
- Prior to placement, alveolar ridge width was assessed by using CBCT or multi-slice CT cross-sectional images.
- Measurements were taken at the crest and at 2mm sections up to 12mm below the crest.
- All implant sites presented with buccal bone thickness of <1mm after implant placement.
- Intra-oral radiographs were taken at the time of implant placement, functional loading, and follow-up intervals of one, two, three, five, and 10 years.
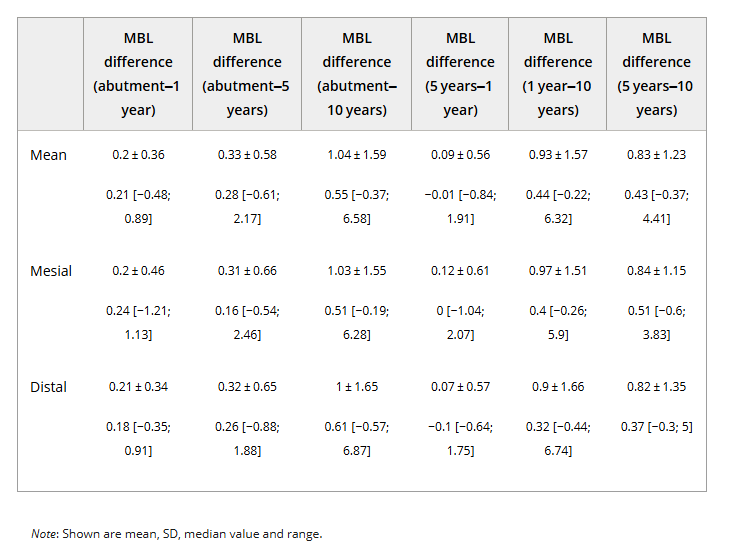
- Marginal bone-level changes were measured by assessing the distance between the implant shoulder and the first visible bone-to-implant contact both mesially and distally.
- Thread pitch distance and total implant lengths were also recorded.
- Full-mouth periodontal charting was performed, which included: full-mouth plaque score (FMPS), full-mouth bleeding score (FMBS), bleeding on probing (BoP), suppuration on probing (SoP), probing pocket depth (PPD), keratinized tissue width (KTW), mucosal attachment type, presence of peri-mucositis and peri-implantitis.
- Radiographic data were analysed in terms of mean, standard deviation, median, and range.
- Measurements were compared across different time points for mesial, distal, and combined sites.
Results
- The study included 28 patients (three males, 25 females) with an average age of 63.4 years (range: 42–76 years).
- A total of 100 implants were placed in 13 males and 87 females. One patient acquired diabetes, and two patients had a history of radiotherapy outside the head-and-neck region.
- Eighty-eight implants were in the upper jaw, while 12 implants were placed in the lower jaw, mostly localized at the second incisor and second premolar area.
- All the implants were 3.5mm in diameter, with the majority of 13mm (45%) or 11mm in length (33%) (Range: 8-15mm).
- At the final 10-year follow-up, 21 patients with 75 implants without any failures, were evaluated.
- FMPS below 20% was found in 6% of the patients. In 22% of the patients, FMPS was between 20% and 50%, while 7% had FMPS exceeding 50%.
- Regarding FMBS, 11% of the patients had scores below 20%, 22% between 20% and 50%, and 72% above 50%.
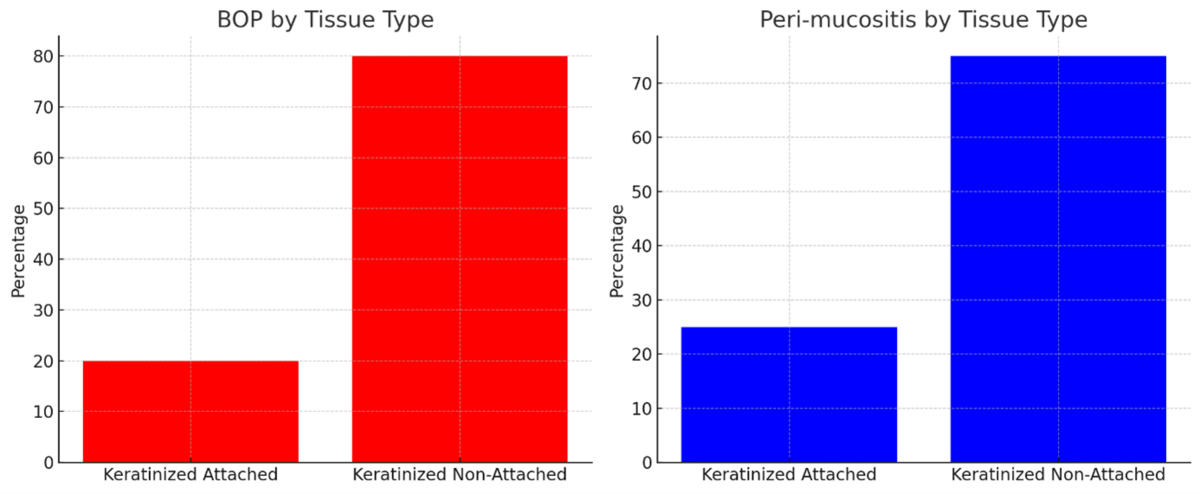
- Implant sites with keratinized but non-attached tissues were more prone to higher BoP values and peri-mucositis presence compared to sites with attached keratinized tissues.
- The overall mean marginal bone loss during the first year of functional loading was found to be 0.2mm ± 0.36. Bone loss measured as 0.18mm, 0.23mm, 0.33mm, and 1.04mm at two, three, five, and 10 years after functional loading, respectively.
Limitations
These successful long-term outcomes, obtained after 10 years of implant placement in narrow bone ridges, may somehow be attributed to the meticulous surgical care, skills, and experience of the surgeon.
A specific set of burs and a single implant system were used, which does not allow generalization of the results.
Information on the fate of the buccal bone in these cases is missing.
- Understanding patient perception is essential for the evaluation of the treatment outcomes and therefore, patient-reported outcomes would have been supporting to the long-term follow-up results.
Conclusions & impact
This 10-year follow-up study demonstrates that oral implants placed in alveolar ridges with limited bucco-oral dimensions (≤4.5mm) achieve successful long-term results with minimal marginal bone loss, revealing a 100% implant survival rate. The findings suggest that meticulous surgical implant placement in narrow ridges without augmentation can be a viable treatment option, particularly in non-aesthetic areas, offering a simplified and cost-effective approach.
This study is valuable as it presents successful 10-year results of implants placed in narrow ridges without augmentation and introduces a classification of peri-implant soft tissues based on keratinization and attachment type. It challenges traditional augmentation needs through a simplified treatment, with reduced costs and patient morbidity.
Rapporteurs: Serra Özdenak and Berfin Sarı, supervised by Professor Bahar Kuru and Associate Professor Ebru Özkan Karaca.
Affiliation: Postgraduate programme in periodontology, Yeditepe University, Istanbul, Turkey.
With kind permission from Wiley Online Library. Copyright © 1999-2024 John Wiley & Sons, Inc. All rights reserved




