
Issue No. 133
Summarised from Journal of Clinical Periodontology, Volume 52, Issue 1, January 2025, 92-101
Editor: Andreas Stavropoulos, chair, EFP scientific affairs committee
CTG versus soft-tissue substitute for contour augmentation at single implants: three-year results
Authors: Lenz Surdiacourt, Véronique Christiaens, Stefanie De Buyser, Aryan Eghbali, Jan Cosyn
Background
Soft-tissue augmentation to increase the mucosal thickness at the buccal aspect of implants aims to re-establish the natural soft-tissue convexity, which is commonly lost after tooth extraction.
Studies have shown that the use of an autologous connective-tissue graft (CTG) results in better aesthetic outcomes, as rated by both professionals and patients, as it at least compensates for the dimensional soft- and bone-tissue changes occurring after tooth loss.
Nevertheless, the use of CTG requires a second surgical site for graft harvesting, which is considered to increase patient morbidity, while in some cases (for example in extended edentulous areas) there might be limited available connective tissue.
Thus, soft-tissue substitutes – most commonly of xenogeneic collagen – have been developed and extensively tested in preclinical and clinical settings, often with seemingly encouraging results.
Aims
The aim of the present study was to report on the three-year outcomes of a randomized control study (Cosyn et al., 2021, 2022), comparing CTG with a particular collagen matrix of xenogeneic origin (CMX) in terms of increase in buccal soft-tissue profile (BSP) at single implant sites with a minor horizontal alveolar defect.
Materials and methods
The present study is a follow-up of patients previously enrolled in a multi-centre RCT comparing the efficacy of CTG and CMX for soft-tissue augmentation at the buccal aspect of single implants. Six experienced and calibrated implant surgeons working in different periodontal practices participated as operators.
The following inclusion criteria were used:
• ≥ 21 years old.
• Good oral hygiene, i.e., full-mouth plaque score ≤25%.
• Presence of a single tooth gap in the maxilla between teeth 15 and 25.
• Both neighbouring teeth present.
• Tooth extraction at least three months before implant installation.
• ≥5mm of keratinized mucosa at buccal aspect of the single tooth gap.
• Class I defect at the single tooth gap, clinically assessed.
• Bucco-palatal bone dimension ≥6mm at the central and crestal aspect of the gap, assessed by CBCT.
The following exclusion criteria were used:
• Systemic diseases.
• Smoking.
• Periodontal disease.
• Untreated caries lesions.
• Need for horizontal bone augmentation at the time of implant placement.
Treatment procedures
Implants were installed after full-thickness mucoperiosteal flap elevation and using a surgical guide. After implant installation, patients were block-randomized to receive either (control group) an autogenous CTG harvested from the palatal mucosa in the premolar region using the single incision technique or (test group) a CMX (Geistlich Fibro-Gide, Geistlich Pharma AG),
The size of the CTG and the CMX was adapted to fit the defect and it was positioned in the buccal envelope and secured with two single sutures onto the buccal mucosa. A screw-retained provisional restoration was then placed, and tension-free primary wound closure was achieved. Sutures were removed after two weeks. The provisional crown was replaced with a permanent crown after three months.
Assessment and outcomes
Intra-oral scans containing an area of interest (AOI) at the buccal aspect of the alveolar ridge at the experimental site: from 0.5mm below the soft -tissue margin to 4mm apically, and extending from the mesial to distal line angle of the implant crown, were assessed at the following time points: T0 (pre-op), T1 (immediately post-op), T2 (3 months), T3 (1 year), and T4 (3 years) by a single blinded examiner. Mean volumetric changes were calculated by software and divided by the size of AOI to determine the mean linear increase in BSP.
Patients’ aesthetic satisfaction was assessed using a visual analogue scale (VAS) with “most unsatisfied” and “most satisfied” positions as extremes, while biological or technical complications occurring between one- and three-year follow-up were also recorded. Presence and extent of recession at the buccal aspect of the implant and the Pink Esthetic Score (PES) were recorded, while the proportion of implants showing peri-implant mucositis and peri-implantitis at three years after surgery was also assessed.
Marginal bone loss from one to three years post-op was assessed on calibrated peri-apical radiographs at the mesial and distal aspects of each implant, and the presence/absence of plaque and bleeding on probing at four sites around the implant was recorded at one and three years.
Results
At three years post-op, 50 of the 60 originally included patients could be examined.
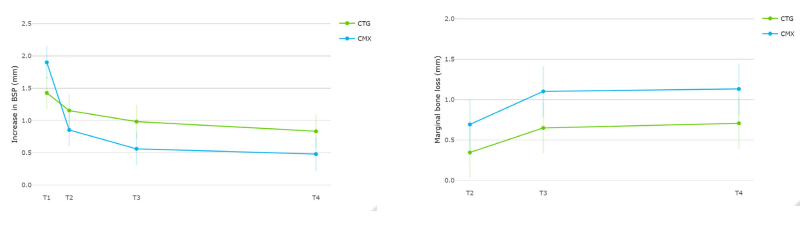
- There was a significant estimated mean difference of 0.35 mm (95% CI: 0.06–0.65) in favour of the control group regarding increase in BSP over time.
- No significant differences between the groups could be observed in terms of patients’ aesthetic satisfaction, midfacial recession, PES, mucosal scarring index, plaque, bleeding on probing, and probing depth.
- Significantly larger marginal bone loss (interproximal) was observed in the CMX group compared with the CTG group (1.13mm vs. 0.71mm, respectively).
- At 3 years post-op, 10 implants in the control group and seven implants in the test group showed peri-implant mucositis, while none of the implants in the control group, but two implants in the test group, suffered from peri-implantitis.
Limitations
- Absolute differences in millimetres do not capture the relative increase in BSP and its relevance for the specific size.
- Patients are in general less critical regarding aesthetic outcomes and significant differences may be irrelevant.
- No estimation of the buccal bone level was performed. This seems relevant information considering the significantly larger interproximal bone loss observed in the test group.
Conclusions
- CTG was more effective in increasing the buccal soft-tissue profile and was associated with less interproximal marginal bone loss compared with CMX at three years post-operatively.
- CTG remains the “gold standard” to increase soft-tissue thickness at the buccal aspect at single implant sites.
Summarized by Andreas Stavropoulos, Chair of the EFP Scientific Affairs Committee
With kind permission from Wiley Online Library. Copyright © 1999-2025 John Wiley & Sons, Inc. All rights reserved




