
Issue No. 135
Summarised from Journal of Clinical Periodontology, Volume 52, Issue 3, March 2025, 484-497
Editor: James Deschner, chair, EFP scientific affairs committee
Mind the gap: Does vertical distance between implants matter?
Authors: Jiayu Gao, Yang Yang, Xingmei Yang, Xuemei Tang, Yili Qu, Yingying Wu, Lin Xiang, Yi Man
Background
Dental implants have been shown to be an excellent replacement for missing teeth. Successful implant treatment largely depends on various patient and local factors, such as implant placement depth, implant abutment geometry, loading time, adequate primary stability, smoking, periodontitis history, and general health.
When placing multiple implants, the horizontal distance between implants can have an impact on inter-implant bone resorption, with the literature suggesting that <3mm of distance between implants leads to an increase in vertical alveolar bone resorption.
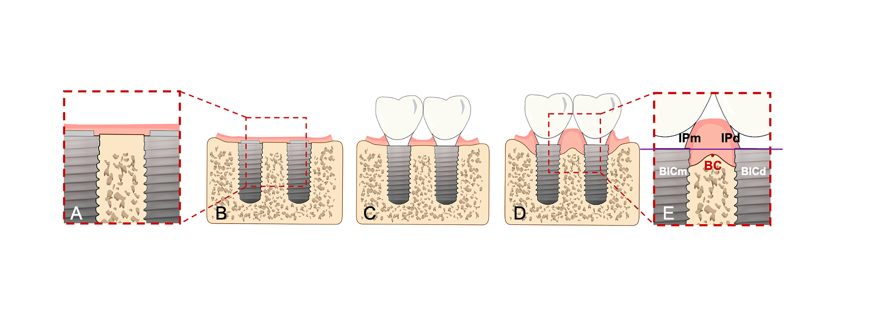
In relation to the vertical implant position, when placed adjacent to natural teeth, a height difference of >3mm between the implant platform and the cementoenamel junction (CEJ) tends to exhibit an increase in bone resorption. At present, there is insufficient evidence in relation to the vertical distance between adjacent implant platforms.
Aim
To investigate the impact of different vertical inter-implant distances (VID) on the long-term success of two adjacent single-unit implants.
Materials and methods
- Study: A retrospective cohort study, analysing 290 patients with 376 adjacent single-unit posterior implants with follow-up of between one and eight years.
- VID groups: Implants were divided into Group 1 (VID <2mm) and Group 2 (VID ≥2mm). Subgroups based on horizontal inter-implant distance (HID <3mm or ≥3 mm) were also analysed.
- Inclusion criteria: Patients with adjacent posterior single-unit implants placed simultaneously, with baseline and follow-up radiographs more than 12 months after prosthesis delivery.
- Exclusion criteria: Implant sites with prior implant failure, inter-implant angles >15°, or implants intended for bridge restorations.
- Clinical protocols: Implants were pre-planned virtually. Bone-level implants were placed with standard surgical protocols, and a bone substitute (Bio-Oss®) was used when required. Submerged healing was allowed for between three and six months prior to second-stage surgery. Annual implant-maintenance visits were completed.
- Radiographic assessment: CBCT and periapical radiographs were used to measure VID, HID, buccal bone thickness, marginal bone loss (MBL), and crest bone loss (CBL). ImageJ software ensured standardised measurements.
- Statistical analysis: Mixed-effects Cox models and generalized linear mixed models accounted for patient-level clustering. Variables included implant positioning, surface treatment, crown retention type, and systemic factors. Post hoc power analysis revealed a power of 65% at a 90% confidence level.
Results
- A total of 376 two-unit adjacent implants from 290 patients were analysed: 223 patients with 280 implant units of VID <2mm (Group 1) and 89 patients with 96 implant units having VID ≥2mm (Group 2). Group 2 had a significantly higher percentage of male patients and more implants placed in the maxilla. Group 1 showed a higher frequency of coronally placed distal implants and lower crown-to-implant ratios.
- Although implant survival was slightly better in Group 2 (96.8% vs. 93.2%), the difference was not statistically significant. Risk factors for implant failure included coronal placement of distal implants and mandibular placement, while longer implants and parallel inter-implant angulation were protective.
- Complication-free survival rates were similar between groups, and peri-implantitis rates did not differ significantly. Cemented crowns that preserved access to the screw significantly reduced implant complications and bone loss. Bone loss—both marginal and crestal—was higher in Group 1, with loss of more than 0.5mm more common in this group.
- LASSO regression identified implant surface, crown retention type, marginal fit, and systemic disease as key predictors of marginal bone loss. Cemented crowns with screw access were associated with reduced bone loss compared to standard cemented crowns.
- Overall, neither vertical implant distance nor horizontal implant distance had a significant impact on implant complications or bone loss in multivariable models.
Limitations
- Reliance on retrospective data introduces inherent recall and reporting limitations, particularly in terms of potential underreporting or misclassification of clinical events increasing selection/information biases.
- Alignment of peri-apical radiographs and CBCT images introduces a source of magnification/angulation error.
- Follow-up radiograph did not utilize individual radiographic jigs but used stock parallelling devices that introduce alignment error.
- The unequal distribution of horizontal inter-implant distances between the two main groups may have affected comparability.
- Most adjacent implants did not exhibit significant platform height discrepancies, which led to their categorization into a 2mm grouping to ensure balanced sample sizes; using a 3mm threshold would have caused an uneven distribution.
Conclusions and impact
- There were no significant differences between the VID groups regarding implant survival (93.2% vs. 96.8%), complication-free survival (60.6% vs. 65.6%), peri-implant disease, or bone loss outcomes.
- HID of <3 mm or ≥3 mm did not influence clinical or radiological outcomes.
- Cemented crowns that allow screw access reduce the risk of CBL ≥0.5mm and MBL ≥0.5mm compared to traditionally cemented crowns.
- Longer implants and a more parallel inter-implant angle were linked to a protective effect against implant failure.
This study implies that dentists potentially may not need to perform extensive vertical bone augmentation or position the implants deeper into the bone if there is a significant height difference between the implants. This could simplify treatment planning for patients with uneven bone levels while maintaining good long-term success for the implants.
Rapporteurs: Eamonn Donohoe, Rawan Kahatab, and Daniel Merrick supervised by Lewis Winning and Ioannis Polyzois.
Affiliation: Postgraduate programme in periodontology, University of Dublin, Trinity College Dublin, Ireland.
With kind permission from Wiley Online Library. Copyright © 1999-2025 John Wiley & Sons, Inc. All rights reserved




