Issue No. 136
Summarised from Journal of Clinical Periodontology, Volume 52, Issue 4, April 2025, 575–588
Editor: James Deschner, chair, EFP scientific affairs committee
Ti‐reinforced PTFE mesh with or without collagen membrane?
Authors: Istvan A. Urban, Matteo Serroni, Debora R. Dias, Zoltán Baráth, Andras Forster, Tiago G. Araújo, Muhammad H. A. Saleh, Alessandro Cucchi, Andrea Ravidà
Background
Vertical ridge augmentation (VRA) is used to rebuild bone in the vertical dimension in areas with significant bone loss. Techniques such as guided bone regeneration (GBR), distraction osteogenesis, and bone blocks are commonly applied.
GBR using titanium-reinforced dense-polytetrafluoroethylene (PTFE) membranes or meshes has shown promising results, but a high risk of healing complications has been described.
Perforated titanium-reinforced PTFE meshes have recently been introduced. These aim to improve the blood supply to the graft by allowing better interaction with the surrounding soft tissue. While this may benefit healing, perforations can also reduce the mesh’s ability to prevent the soft tissue from invading the grafted area. To counteract this, clinicians may opt to cover the mesh with a collagen membrane.
Although early studies have reported high bone fill and few complications with this approach, the additional cost of a collagen membrane is a consideration. The current study was designed to assess whether the mesh alone can achieve comparable outcomes to the combination of mesh and membrane.
Aim
This clinical study aimed to evaluate whether using a perforated titanium‐reinforced PTFE mesh alone is non-inferior to the same mesh covered with a native collagen membrane in achieving vertical bone gain. Secondary outcomes related to volumetric changes and clinical outcomes including complications.
Materials and methods
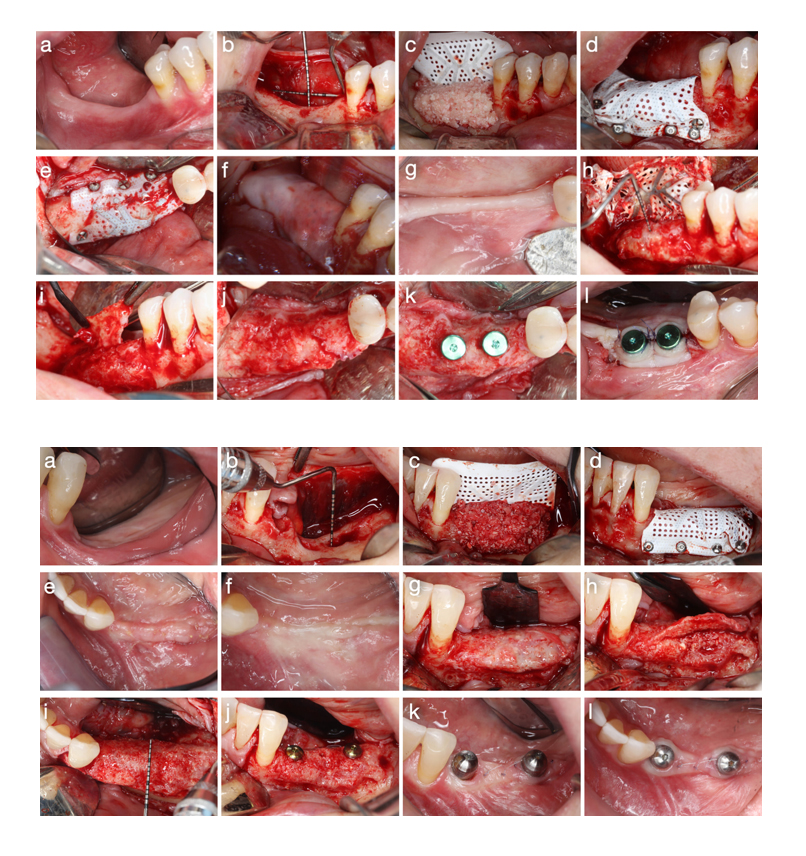
- Design: A parallel, non‐inferiority, single-centre randomized controlled trial.
- Participants: 30 partially edentulous patients who required vertical (>1mm) and horizontal ridge augmentation for late implant placement in at least one tooth site in the maxilla or mandible. Heavy smokers (>10 cigarettes/day) were excluded.
- Randomization: Patients were randomly assigned (15 per group) to one of two treatment arms using a computer-generated table. A sealed envelope was opened and revealed the treatment group to the surgeon after the PTFE mesh was stabilised. Patients, radiographical examiners, and the study analyst were blinded.
- Interventions:
- PTFE group: Received a bone-graft mixture (autogenous bone chips combined with deproteinized bovine bone mineral in a 1:1 ratio) covered with a stabilized and perforated titanium‐reinforced PTFE mesh.
- PTFE + CM group: Received the same bone-graft mixture and stabilized PTFE mesh, which was subsequently covered with a native collagen membrane, without additional fixation.
- Surgical protocol:
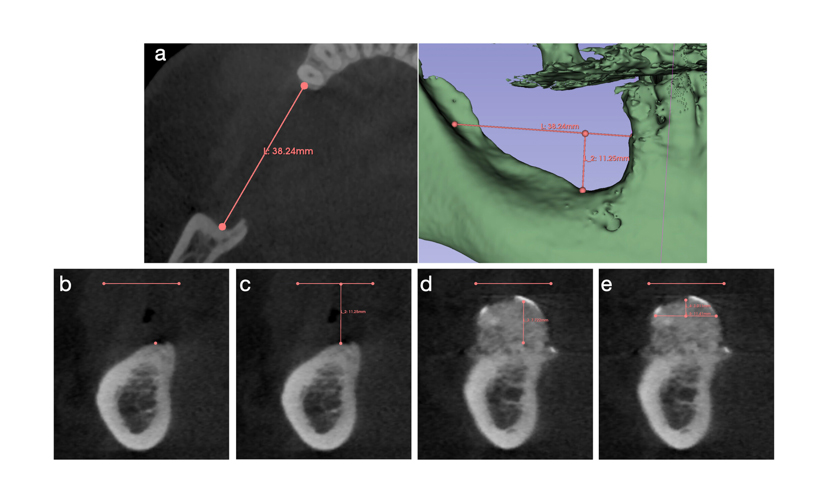
- Preoperative CBCT was performed to assess defect dimensions.
- Standardized full-thickness flap designs, vertical and horizontal measurements, cortical perforations, and fixation of the mesh using titanium pins/screws.
- All patients received systemic antibiotics and were reassessed at the same timepoints.
- Outcome measures:
- Primary: Absolute vertical bone gain (VBG) assessed via superimposed CBCT reconstructions after nine months.
- Secondary: Relative vertical bone gain, horizontal bone gain, augmented and regenerated bone volumes, bone density, incidence and nature of complications, evaluation of pseudo-periosteum type, ability to place implants in a prosthetically driven position, need for additional bone augmentation.
Results
- Vertical bone gain:
- Absolute VBG was on average 4.47mm in the PTFE group and 4.11mm in the PTFE + CM group. Non-inferiority was not shown. Superiority analysis revealed that the difference was not statistically significant.
- Relative VBG was 79.2% in the PTFE group and 85.8% in the PTFE + CM group. Non-inferiority was not shown. Superiority analysis revealed that the difference was not statistically significant.
- Horizontal bone gain: Comparable between groups: average of 10.3mm (PTFE group) versus 9.7mm (PTFE + CM group).
- Volumetric measurements:
- Augmented bone volume (i.e., all the regenerated tissue under the mesh; ABV) tended to be higher in the PTFE group (~2230mm³ vs. ~1595 mm³), while regenerated bone volume (i.e., only the newly formed mineralized bone tissue; RBV) similarly favoured the PTFE group, though the level of significance was not reached.
- The difference between ABV and RBV, defined as lacking bone volume (LBV), represented non-mineralized pseudo-periosteum and it was significantly higher in the PTFE group.
- Pseudo-periosteum: A higher frequency of type 1 pseudo-periosteum (minimal soft-tissue interference) was observed in the PTFE + CM group, suggesting better protection against soft-tissue ingrowth.
- Complications and bone density:
- Both groups demonstrated low complication rates (6.7% in both groups).
- Bone density assessments revealed similar proportions of medium- and high-density outcomes in both treatment groups.
- Implant placement: Adequate bone volume in all cases allowed prosthetically guided implant placement without the need for additional bone augmentation.
Limitations
- As this RCT is the only study evaluating a perforated PTFE mesh with a native CM, direct comparison with previous research is not feasible.
- The variability in the location of the analysed defects may introduce anatomical and technical factors that influence outcomes.
- The short-term follow-up does not allow assessment of implant survival or long-term peri-implant bone loss.
- The pseudo-periosteum was measured with a periodontal probe, which may be considered an inaccurate method given a probe’s 1mm measurement margin of error. This limitation holds true despite standardization efforts.
- All surgeries were performed by one very experienced surgeon. Therefore, the external validity of the results of this study is limited.
Conclusions and impact
- Non-inferiority of PTFE alone compared with PTFE + CM was not demonstrated for absolute and relative vertical bone gain, and significant differences could not be demonstrated on the basis of superiority analyses.
- Both techniques showed similarly low complication rates.
- The addition of a collagen membrane was associated with a higher incidence of type 1 pseudo-periosteum and less LBV, suggesting enhanced control of soft-tissue ingrowth.
- The findings indicate that while both methods are clinically acceptable, the collagen membrane may offer a protective benefit that optimizes the quality of regenerated bone, although at a higher cost.
- The cost-benefit ratio of using two membranes needs to be shown by future studies.
The study suggests that both PTFE mesh approaches can achieve reliable vertical ridge augmentation. The use of a collagen membrane may better prevent soft-tissue invasion, potentially improving the outcome of bone regeneration. Whether the additional cost of a collagen membrane outweighs the benefit is yet to be shown.
Rapporteur: Matthijs Hindryckx, supervised by Jan Cosyn.
Affiliation: Postgraduate programme in periodontology, Ghent University, Belgium.
With kind permission from Wiley Online Library. Copyright © 1999-2025 John Wiley & Sons, Inc. All rights reserved