Prevention & Public health, Public health & Prevention, Article
The economic impact of periodontitis in Switzerland: estimating potential healthcare savings
15 May 2023
In 2021, the EFP commissioned a report from the Economist Intelligence Unit (EIU) on the socioeconomic impact of periodontitis, which provided a comprehensive analysis of the financial and human cost of gum disease in six Western European countries. Christoph Ramseier, of the University of Bern, has sought to apply the same model to Switzerland, assessing the economic impact of periodontitis and how a prevention-based healthcare strategy could lead to substantial savings by individuals and the state as well as improved general health.
Periodontitis has been linked to several systemic health conditions, including diabetes and cardiovascular disease, but the economic impact of periodontal disease has not been adequately addressed in many countries, including Switzerland.
Given the significant burden that periodontal disease places on both oral and general healthcare systems, it is crucial to understand its impact on public health and the economy, particularly in countries where such data are scarce or non-existent.
In an effort to address the economic impact of periodontitis, the EFP commissioned the report Time to take gum disease seriously: the societal and economic impact of periodontitis from the EIU, the research and analysis division of the Economist Group. The report, sponsored by Oral-B and published in June 2021, estimated the potential cost benefits of periodontal treatment in the healthcare systems of six European countries: France, Germany, Italy, the Netherlands, Spain, and the UK.
The report highlighted the importance of treating periodontal disease to reduce oral-healthcare costs and improve the quality of life of those affected. As this study did not include Switzerland, there was a need for further research in the Swiss context to improve our understanding of the economic impact of periodontitis and the potential cost savings associated with its treatment.
Applying the model to Switzerland
We attempted to fill this gap in the literature by estimating the cost savings of periodontal treatment in Switzerland, not only for the oral-healthcare system but also for the entire healthcare system. This broader perspective is essential, because it allows a more comprehensive understanding of the economic impact of periodontitis and the potential benefits of investing in its prevention and treatment.
Our analysis considers both the direct costs associated with periodontal care and the indirect costs of non-communicable diseases (NCDs) that are related to periodontal disease, such as diabetes and cardiovascular disease.
Switzerland, with its unique healthcare system and high standard of living, provides an interesting context for this research. The Swiss healthcare system is characterised by universal coverage, a decentralised structure, and a variety of insurance providers. In addition, the country's high average income and strong social safety nets create an environment in which the financial burden of chronic diseases such as periodontitis can be more accurately assessed.
In Switzerland, periodontal treatment and supportive periodontal care are generally paid for “out-of-pocket” – that is, directly by patients.
By focusing on the Swiss context, our study contributes to the growing body of literature on the economic and societal impact of periodontitis and provides valuable insights that can inform health-policy decisions and resource allocation.
Swiss general-health expenditure has increased by 3.7% per year since 1995, reaching CHF82.5 billion (€84.1 billion) in 2017. It is estimated that it could increase to CHF155 billion by 2040. Dental costs the country reached CHF4.2 million (€4.28 million) in 2020, while the total cost of periodontitis in Europe was estimated at €158.6 billion in 2018 (Bothelo et al. 2022).
The aim of our study was to estimate the direct and indirect costs of treating gingivitis, periodontitis, and related NCDs in Switzerland. A simulation model was used to examine whether professional periodontal care reduces healthcare costs. The model was based on the economic model used in the EIU report for the EFP, which assessed the financial impact on oral-healthcare costs of treating and preventing gingivitis and periodontitis in the six countries studied.
Estimating the lifetime costs of periodontitis for Swiss citizens
The simulation considered three types of periodontitis: mild, moderate, and severe and the model used in the EIU report was adjusted to derive transition probabilities from general prevalences in the Swiss population. The simulated individuals were aged from 35 to 100 years’ old and were divided into younger (35-64) and older (65-100) groups. The only difference between the groups was the prevalence of periodontal disease, which was higher in the older group. The simulation included different disease states and treatment steps, which were adopted and expanded from the EIU study.
Three scenarios were simulated with different prevalences for the age groups, representing different levels of dental-hygiene visits and improvements in disease and prevention information. The study also included out-of-pocket and social welfare-funded costs directly related to periodontitis treatment, as well as indirect costs from treating NCDs.
The simulation and statistical analyses were performed using RStudio software, with 200,000 simulated individuals included to ensure an accurate estimation of means and quantiles.
The power of prevention
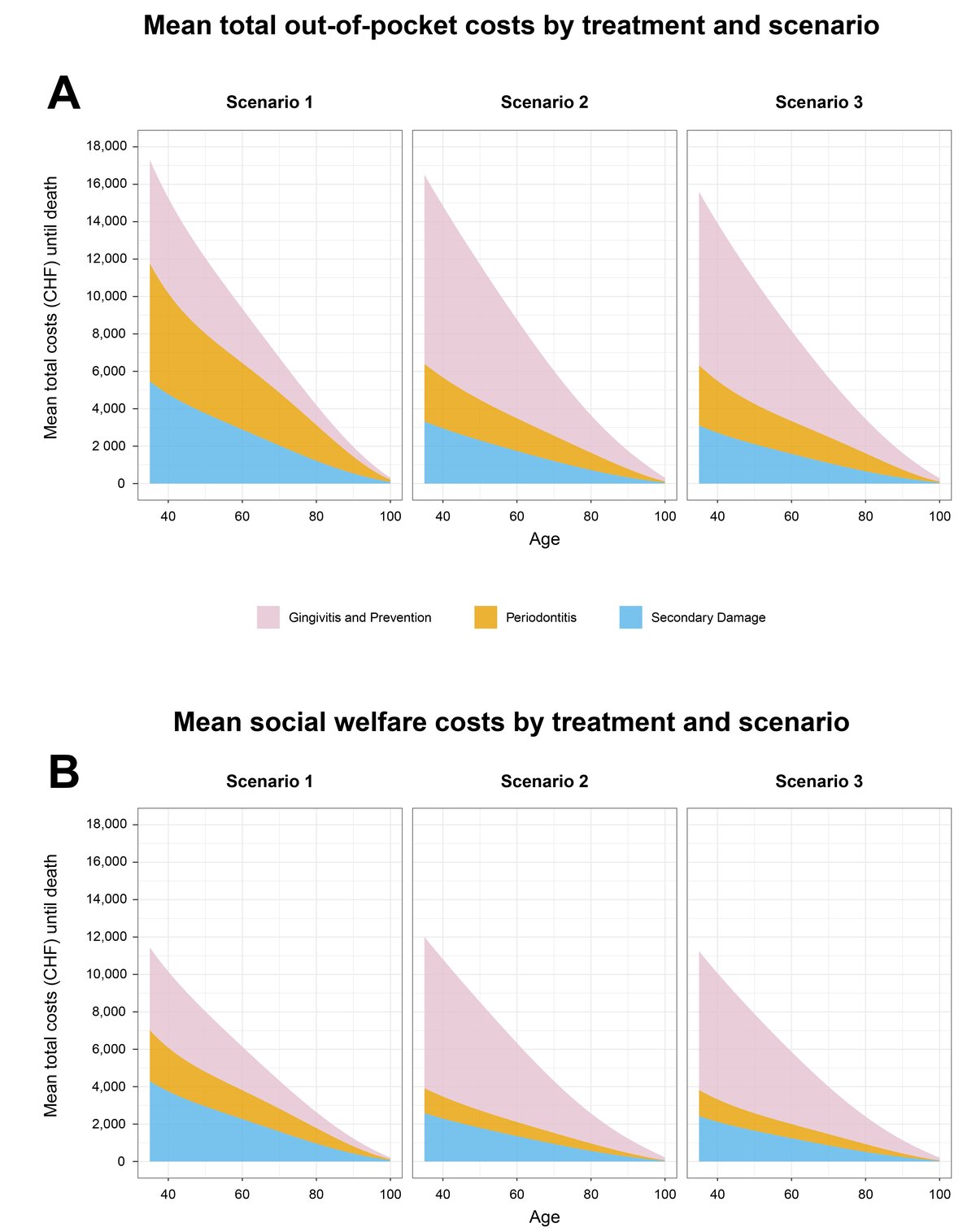
The average total cost of treating gingivitis, periodontitis, and associated secondary damage from NCDs in Swiss citizens aged 35 to 100 years was analysed under three different scenarios. In each scenario, the costs were divided into out-of-pocket costs and costs paid by the social-welfare system.
- Scenario 1: One prophylactic appointment per year for patients with gingivitis (current situation).
- Scenario 2: Two prophylactic appointments per year for patients with gingivitis, leading to a better early detection of periodontitis and a reduction in overall treatment costs.
- Scenario 3: One prophylactic appointment per year for healthy patients and two appointments per year for patients with gingivitis, leading to a reduction in overall treatment costs. In this scenario, patients are also given more information about the disease and its prevention.
The highest average out-of-pocket costs were found in scenario 1, followed by scenario 2, while scenario 3 had the lowest expected total costs for all age groups.
A different trend was observed for the costs paid by social welfare, with the highest average amounts generated for scenario 2, followed by scenario 1 up to the age of 69. After this age, the order was the same as for out-of-pocket costs.
When the costs were examined by type of treatment, it was found that out-of-pocket and social-welfare costs for the treatment of periodontitis and secondary damage from NCDs accounted for over 60% of all expected lifetime costs in scenario 1. In scenarios 2 and 3, the costs of treating periodontitis and secondary damage were halved, and the costs of treating gingivitis increased significantly, accounting for up to 60% (out-of-pocket) and about 66% (social welfare) of all costs.
The return on investment (ROI) was calculated by comparing the total costs for the current Swiss population aged 35 to 100 years under each scenario. The total costs for this population were highest in scenario 1, and the ROI was CHF2.6 billion for scenario 2 and CHF5.9 billion for scenario 3.
This suggests that, on average, individuals could save up to CHF500 under scenario 2 and more than CHF1,100 under scenario 3 over their lifetime. In terms of total costs paid by the social-welfare system, the differences were smaller, with a negative ROI for scenario 2 and a positive ROI of CHF1.0 billion for scenario 3.
Overall, appropriate diagnosis and adherence to professional periodontal care at the individual level – as assumed in scenario 3 – can reduce total costs by approximately CHF1,700 per person.
While the total cost of prevention for the individual under this scenario increases by about CHF3,750, the total cost of treating periodontitis decreases by CHF3,100 and the cost of treating secondary damage decreases by CHF2,350 – an overall saving of CHF1,700. Assuming that a Swiss citizen in Scenario 3 has an average of 100 periodontal care visits, a total of CHF17 in healthcare costs can be saved for each dental and dental-hygiene visit.
How to unlock billions in savings
The impact of enhancing oral healthcare and periodontitis prevention amounts to substantial savings both in out-of-pocket and social-welfare costs.
The simulation emphasises early disease detection and prevention of gingivitis to reduce periodontitis and its costs. By halving periodontitis prevalence and improving gingivitis management, the Swiss population could save CHF2.61 billion to CHF5.94 billion in out-of-pocket expenses and up to CHF1.03 billion in social welfare costs. The study also highlights that the early onset of periodontal disease in adults leads to increased secondary damage and a greater healthcare burden. Moreover, our results emphasise the need for early detection, gingivitis prevention, and effective treatment in reducing the direct and indirect costs of periodontitis, saving between CHF2.6 billion and CHF5.9 billion in out-of-pocket costs and up to CHF1.0 billion in social-welfare expenditure.
This simulation is consistent with other studies examining the impact of periodontal therapy on NCDs and healthcare costs. The EIU report for the EFP suggested that the most beneficial scenarios are to eliminate gingivitis and increase the diagnosis rate of periodontitis by 90% through early detection, treatment, and improved oral care at home.
Limitations of our study include the potential underestimation of cost savings because of conservative assumptions, the absence of age groups below 35 years, and the exclusion of Stage IV periodontitis. However, the study highlights the importance of integrating general and dental healthcare to manage comorbidities and suggests that Switzerland should prioritise the prevention of gingivitis, promote early diagnosis of periodontitis, and raise awareness of its impact on NCDs and the healthcare system.
Like the EIU study for the EFP, this research about Switzerland helps lobbying at national and European Union level because it provides clear data that show how prevention is the key to cutting healthcare expenditure.
Select bibliography
Time to take gum disease seriously: The societal and economic impact of periodontitis, The Economist Intelligence Unit, 2021. Commissioned by the European Federation of Periodontology and sponsored by Oral-B.
Christoph Ramseier, Raji Manamel, Raffael Budmiger, Norbert Cionca, Philip Sahrmann, Patrick Schmidlin, Lukas Martig. (2022). Cost savings in the Swiss healthcare system resulting from professional periodontal care. Swiss Dent J 132: 764-779 (2022).
João Botelho, Vanessa Machado, Yago Leira, Luís Proença, Leandro Chambrone, José João Mendes. (2022) Economic burden of periodontitis in the United States and Europe: An updated estimation. J Periodontol 93: 373-379 (2022).
Reproducibility and further improvements: All code utilised in this simulation is openly available on the website of the Swiss Dental Journal, inviting researchers from additional countries to reproduce, enhance, and engage in further discussions surrounding this simulation.
https://github.com/significantis/perio-tx-and-health-care-costs-simulation

Biography
PD Dr. med. dent. Christoph A. Ramseier is a Swiss periodontist who received his education and training at the University of Bern. He earned his dental degree in 1995 and his doctorate in dental medicine in 2000. From 1999-2000, he underwent specialised training in periodontology and implantology at the University of Bern, where he became a board-certified specialist in periodontology by the Swiss Society of Periodontology (SSO/SSP) and the European Federation of Periodontology (EFP) in 2004. From 2004-2008, Dr. Ramseier was a research fellow at the University of Michigan, and in 2016 he became a private docent at the University of Bern, where his research focuses on periodontal risk management and supportive periodontal care.





