Publications Hub, EuroPerio, Treatment, Article
What are the choices for clinicians when moving to Step 3 of periodontal therapy?
19 March 2025
Ahead of the EuroPerio11 session on 'Controversial issues in non-surgical periodontal therapy', which will consider various approaches to Step 3 of periodontal therapy, debate moderator Nurcan Buduneli and speakers Cristiano Tomasi and Alexandra Staehli consider the issues.
The EFP clinical guidelines on the treatment of stage I-III periodontitis propose a stepwise approach to the therapy with an increment in terms of intervention between steps. Before moving to the next step, the goals of the previous one have to be verified by clinical re-evaluation, writes Nurcan Buduneli.
Step 2, non-surgical subgingival mechanical instrumentation, is an effective means to treat and close the majority of periodontal pockets in most patients (≤4mm probing pocket depth without bleeding on probing).
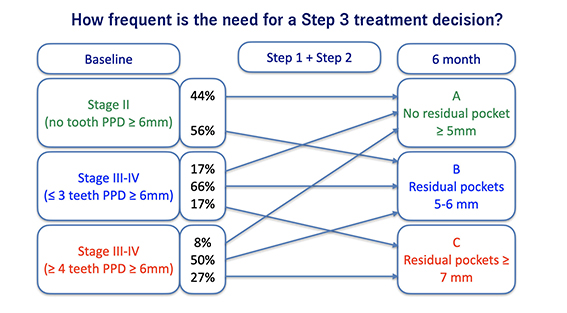
However, in periodontitis patients, teeth with deep pockets (probing depth ≥6mm) or complex anatomical surfaces may prevent the complete removal of subgingival biofilm and calculus. Therefore, some sites may require further treatment to achieve the goal of pocket closure.
The individual response to the second step of therapy should be assessed after an adequate healing period and, if required, potential approaches to Step 3 of periodontal therapy include photodynamic therapy, the use of lasers, and non-surgical re-instrumentation.
How effective is non-surgical re-instrumentation as Step 3 of periodontal therapy?
An interview with Cristiano Tomasi
What are the indications that would suggest non-surgical retreatment of residual pockets as Step 3 of periodontal therapy, rather than opt for other approaches (laser, antimicrobials, photodynamic therapy, etc)?
Given that the patient has fulfilled requirements of Step 1, thereby reaching an adequate level of self-performed supra-gingival infection control and possibly reducing modifiable risk factors, we should carefully evaluate site-level characteristics to understand the potential benefit of a non-surgical re-instrumentation. The additional use of the devices mentioned have not proven a clear benefit and a favourable cost-benefit ratio in Step 3. The presence of an angular bony defect or a horizontal furcation involvement are indicators of the need for a surgical approach.
What is the difference between using hand instrumentation alone, ultrasonic instrumentation alone, and using both hand and ultrasonic instrumentation?
The results of a study we recently published [1] suggest that a combined use of both hand and ultrasonic mechanical instrumentation on the subgingival root surface increases the probability of achieving the desired treatment goal, which is pocket reduction to 4mm or less.
What percentage of patients who receive non-surgical retreatment as Step 3 of periodontitis therapy achieve acceptable outcomes?
That is a very interesting question. In our latest study, after the first two steps 57% of patients had no residual deep pockets and 16% of patients had no residual pocket deeper than 4mm. Performing non-surgical retreatment improved the status of around 10% of patients with residual pockets, increasing the percentage of patients with no residual pocket deeper than 4mm to almost 20%. One third of patients still presented deep residual sites, which calls for additional treatment. It should be noted the risk of recurrence was 2.7 times higher in smokers than in non-smokers, and that, among smokers, the probability of resolution of the disease after retreatment was half compared to non-smokers.
Are the results of the non-surgical retreatment of residual pockets different in relation to different types of tooth and the presence of furcation involvement, bony defects, etc?
Yes. We have seen in our studies that these are both significant factors that affect the outcome at site level. The presence of one or more of these charcteristics has to be considered when planning further treatment procedures.
What are the main factors that might influence the effectiveness of surgical retreatment?
That is a difficult one. First of all, we should clarify which surgical approach we are discussing. For example, in case of a regenerative procedure we know that the surgical technique may play an important role, given that patient-related factors are under control.
In what circumstances might it be better not to adopt non-surgical treatment as Step 3 and move directly to surgical intervention?
In general, I would say we should proceed when we have evidence that we have already achieved all possible benefits from non-surgical instrumentation. However, we should not forget to conduct a cost-benefit evaluation and consider the strategic value of the tooth as determined through careful treatment planning.
[1] Anna Liss, Kajsa H. Abrahamsson, Maria Welander, Cristiano Tomasi (2025). Effectiveness of nonsurgical re-instrumentation of residual pockets as step 3 of periodontal therapy: A field study. Journal of Periodontology. Online version before inclusion in an issue. https://doi.org/10.1002/JPER.24-0532
Can lasers improve outcome of non-surgical therapy?

By Alexandra Staehli
Periodontal disease is triggered by a dysbiotic biofilm, leading to a disrupted host immune response and, ultimately, the destruction of periodontal tissue. Mechanical biofilm removal remains the standard form of care, primarily through non-surgical subgingival instrumentation using manual curettes and ultrasonic devices.
However, non-surgical therapy with hand and power-driven instruments presents challenges—particularly in anatomically complex sites such as furcations, deep intrabony defects, and other intricate root morphologies. In such areas, laser beams may provide improved access to calculus and deposits, potentially enhancing decontamination.
My presentation at EuroPerio11 will summarize the outcomes of laser applications in periodontal therapy. First, it will address key questions such as which lasers have been tested for subgingival instrumentation and what their technical protocols entail. The treatment outcomes using lasers will then be compared with those achieved with conventional scaling and root-planing protocols.
A recent randomized controlled trial [1] demonstrated superior results for adjunctive laser therapy compared to scaling and root planing alone, which remains the current “gold standard”. However, findings across various studies remain controversial and the heterogeneity of laser types and treatment protocols undoubtedly complicates direct comparisons.
In contemporary research, patient-specific factors and tailored treatment protocols are being explored across various fields. Could this also apply to laser therapy?
[1] Codruta Elena Ciurescu, Norbert Gutknecht, Vlad Alexandru Ciurescu, Anca Gheorghiu, Rene Franzen, Nicole B. Arweiler, Anton Sculean, Raluca Cosgarea (2021). Two-year outcomes following the adjunctive use of InGaAsP and Er,Cr:YSGG lasers in nonsurgical periodontal therapy in patients with stages III and IV periodontitis. Quintessence International, 52(10), 848–861. https://doi.org/10.3290/j.qi.b1702285.
Biographies



Nurcan Buduneli is Professor of Periodontology and Chair of the Periodontology Department, School of Dentistry, Ege University, İzmir, Turkey. After graduating from this university's dental school, she did her PhD in the Periodontology Department, followed by postdoctorate research at Copenhagen University in Denmark. She has visited many dental schools in Europe and USA as a guest researcher or visiting professor. Currently an associate editor of Oral Diseases, and section editor of Current Oral Health Reports, she is the author of more than 200 publications, and two books.
Cristiano Tomasi is an associate professor in the Department of Periodontology at the Institute of Odontology, Sahlgrenska Academy, University of Gothenburg. He obtained his DDS from Verona University (1991), and then his specialization in clinical periodontology (2002) and his PhD in 2007 from the University of Gothenburg. He was the winner of the EFP Postgraduate Research Prize in 2005 and of the SSP Young Researcher Prize in 2007. An active member of the Italian Society of Periodontology and Implantology (SIdP) and the Italian Academy of Osseointegration (IAO), he is also a guest professor at the University of Padua in Italy.
Alexandra Staehli completed her postgraduate training in periodontology and implant dentistry at the Department of Periodontology of the University of Bern, Switzerland, in 2015. She later pursued a research fellowship in oral biology at the Medical University of Vienna, Austria, before returning to Bern in 2018 as a staff member in the Department of Periodontology. Her research focuses on clinical studies in periodontal regeneration, as well as the interplay between bacterial biofilms, host response, and therapeutic approaches.
Controversial issues in non-surgical periodontal therapy - a debate EuroPerio11 | Vienna | Thursday 15 May, 10-30-12.00
EuroPerio11 | Vienna | 14-17 May: Information and Registration




