Research, Clinical & Translational Research, Treatment, Article
What happens after healing when keratinised and non-keratinised tissue are transpositioned?
23 July 2024
The EFP recently awarded its Graduate Research Prize 2023, which promotes original graduate research. In the third of a series of articles by the four winners, Andrea Roccuzzo (University of Bern, Switzerland) explores healing after heterotopic mucosa transpositioning at dental implants and teeth.
Previous research has shown mixed findings about what happens with healing and tissue stability around dental implants and teeth. Some studies have shown no difference in healing or tissue stability related to the presence or absence of keratinised tissue (KT), while others have indicated that the peri-implant mucosal seal is more stable when covered by keratinised epithelium. Recent systematic reviews have demonstrated the need for a certain width and thickness of the KT around implants, so it is desirable to maintain a soft-tissue seal with characteristics similar to those around teeth in order to preserve peri-implant health.
Research evaluating the heterotopic transpositioning of the gingiva into the alveolar mucosa has shown that tissue specificities were preserved, revealing the characteristics of their original location, while preclinical models have indicated that the characteristic features of the epithelium are most likely determined by the underlying connective tissue.
However, a very recent experimental study – in which a connective tissue graft (CTG) was placed at teeth and implants after the complete excision of the KT – showed that new KT formed around teeth but not around implants, which is difficult to explain.
At dental implants, it remains unknown to what extent tissue specificities of the KT remain the same following heterotopic transposition into the alveolar mucosa. In this context, our preclinical study sought to evaluate the tissue specificity after heterotopic transpositioning at implants and teeth.
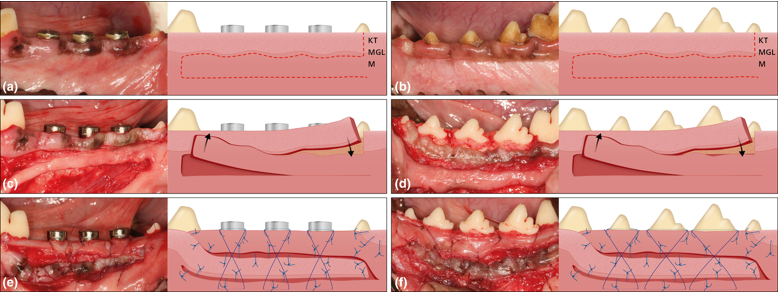
The study, using four female Beagle dogs with healthy and intact dentition, had a split-mouth design: one hemi-mandible with remaining teeth (control) and the other with dental implants (test). Premolars 2, 3, and 4 plus three implants per mandible were evaluated clinically and histologically – a total of 24 sites in the four animals. A 12-week healing period was allowed after the final surgical procedure.
The clinical measurements carried out pre-surgery (T0) and three months afterwards (T1) were:
- Width of the KT (mm)
- Probing pocket depth (PPD, mm)
- Bleeding on probing (BOP, %)
- Probing attachment level (PAL, mm)
- Plaque and calculus (%)
After the taking of the clinical measurements, the dogs were sedated and then sacrificed. Histological procedures and histomorphometric analysis were then carried out.
Following all surgical procedures, healing was uneventful without infections or other complications and all 24 sites were available for further analysis. The results included:
Clinical
- At T1, a certain width of gingiva was re-established at the soft-tissue margin around teeth, but no tissue was formed at the mucosal margin around the implants. Irrespective of the group, the healing resembled, at some locations, scar-like tissues.
- In some cases, both at implants and teeth, the band of KT was maintained where the KT was apically transpositioned into the zone of previously nKM.
- In some cases where the KT was transpositioned apically, scar tissue was visible without obvious signs of keratinization. It may be speculated that the transpositioned flaps were partially lost during the healing.
- The PPDs at both tooth sites and implant sites were reduced, while the soft-tissue reduction from T0 to T1 was higher for implants compared to tooth sites and the PAL loss was statistically significantly greater at the implant sites compared to tooth sites.
Histological
- All implants showed histologically successful osseointegration, with mild inflammation observed in the soft tissues around teeth and implants, and with biofilm and/or calculus formation.
- At the implant sites, the peri-implant mucosal margin after transposition of nKM was characterized by a non-keratinized epithelium, and the non-keratinized zone at implant sites was mostly followed by a zone of KT originating from the transpositioned KT.
- At the tooth sites, a regeneration of the gingival unit was evident at the location of the transpositioned nKM, displaying the characteristics of KT. At a distance from the gingival margin, in most cases the nKM transposition maintained a non-keratinizing epithelium.
- Elastic fibres were absent in the connective tissue below the keratinized epithelium, whereas they were numerous in the connective tissue under the non-keratinized epithelium.
Histomorphometry
- No KT directly at the mucosal margin was detected at any implant site.
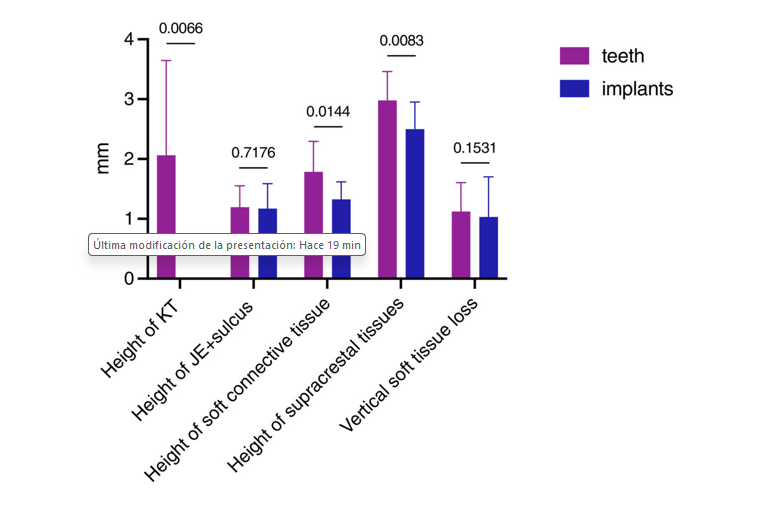
- The height of the junctional epithelium (JE), including the sulcus depth, was similar for teeth and implants.
- The vertical distance of soft connective tissue was statistically significantly higher at tooth compared to implant sites, and the height of supracrestal tissues was larger for teeth than for implants.
- The vertical soft-tissue loss (mucosal or gingival recession) was similar for tooth and implant sites.
First histologic evidence
The findings revealed that, at both teeth and implants, the KT positioned into nKT may result in the formation of KT, thereby confirming the results obtained for teeth in studies by Karring and coworkers published more than 50 years ago. The most significant finding of our study was that, for the first time, histologic evidence was provided for the maintenance of KT characteristics originating from peri-implant locations positioned into nKT.
On the other hand, the heterotopic transpositioning of nKT into a region previously occupied by KT failed to result in the formation of KT at implant sites, while at tooth sites, the formation of a new band of gingiva was consistently observed after heterotopic transpositioning. As keratinization of the mucosa may only be expected in the presence of connective tissue originating from KT, it can be assumed that the induction of KT adjacent to teeth must have come from cells originating
from the periodontal ligament. Our results thus lend further support to the need for soft tissue derived from an anatomical site with KT to induce the formation of a keratinized epithelium.
Our study’s findings indicate that the KT transpositioned into nKT remained unaltered in its morphological characteristics and that the transpositioned Nkt was accompanied by the formation of KT at the tooth but not at implant sites.
This study a milestone publication providing unique histological evidence of extremely high clinical relevance.
This article is based on Jean-Claude Imber, Andrea Roccuzzo, Alexandra Stähli, Dieter D. Bosshardt, Fernando Muñoz, Christoph A. Ramseier, Niklaus P. Lang, Anton Sculean. ‘Clinical and histologic evaluation of heterotopic mucosa transpositioning at teeth and dental implants.’ Clinical Oral Implants Research 2023; 34: 1395-1405. doi:10.1111/clr.14184
Note: The EFP Graduate Research Prize seeks to promote original graduate research, performed within the framework of postgraduate training the federation’s accredited graduate programmes in periodontology. It is awarded annually in two categories: clinical research and preclinical/basic research. It is open to all students of EFP accredited graduate programmes in periodontology.
Bibliography
Karring, T., Østergaard, E., & Löe, H. (1971). Conservation of tissue specificity after heterotopic transplantation of gingiva and alveolar mucosa. Journal of Periodontal Research, 6(4), 282–293. https: //doi.org/10.1111/j.1600-0765.1971.tb006 19.x
Liñares, A., Rubinos, A., Puñal, A., Muñoz, F., & Blanco, J. (2022). Regeneration of keratinized tissue around teeth and implants following coronal repositioning of alveolar mucosa with and without a connective tissue graft: An experimental study in dogs: Fifty years after Karring's landmark study: Fifty years after Karring's 71 landmark study. Journal of Clinical Periodontology, 49, 1133–1144.https://doi.org/10.1111/jcpe.13673
Sculean, A., Gruber, R., & Bosshardt, D. D. (2014). Soft tissue wound healing around teeth and dental implants. Journal of Clinical Periodontology, 41(Suppl 15), S6–S22. doi.org/10.1111/jcpe.12206

Andrea Roccuzzo graduated in dentistry (DDS) from the University of Turin, Italy. He is a specialist in periodontology (SSP and EFP) after completing the EFP-accredited postgraduate programme in periodontology and implant dentistry at the University of Bern, Switzerland. He holds a master’s degree in periodontology and implant dentistry, a PhD in health sciences (dentistry), and a Doctor Medicinae Dentium (Dr. med. dent.) from the same institution. He works as a senior lecturer in the Department of Periodontology at the University of Bern and is actively involved in several pre-clinical and clinical studies.