Therapy, Treatment, Article
Which is best technique for preserving the alveolar ridge after tooth extraction?
31 October 2023
Researchers at the EFP-accredited programme in periodontology at the National and Kapodistrian University of Athens, Greece, have performed a randomised clinical trial (RCT) to compare different techniques for alveolar ridge preservation after tooth extraction. Lead author Iosif El Sioufi presents the results.
A tooth extraction is followed by a sequence of events that lead to alterations in the dimensions of the alveolar ridge, such as a reduction of the width and height of the alveolar crest. The most significant changes take place in the first six months after tooth extraction, with an average bone resorption of 3.79mm horizontally and 1.24mm vertically. This decrease in osseous volume can have a profound impact on implant dentistry and may require the use of bone-augmentation techniques, while aesthetics may be compromised, especially in the maxillary anterior zone.
To compensate for such alterations, an array of alveolar ridge preservation (ARP) procedures has been proposed. In general, these techniques are based on placing a bone graft into the socket, immediately after tooth extraction, and sealing the socket with a barrier. The effectiveness of these interventions has been evaluated in several studies and it has been well documented that ARP procedures result in significantly reduced bone resorption compared to management without ARP. Indeed, the EFP’s XV European Workshop in Periodontology, held in 2018, concluded that, compared to tooth extraction alone, ARP may prevent bone reduction of 1.5-2.4mm horizontal, 1-2.5mm vertical mid-buccal, and 0.8-1.5mm vertical mid-lingual.
Regarding bone-grafting materials, we observe that the most prevalent in the literature are allografts and xenografts. The results from randomised controlled trials (RCTs) demonstrate that both types of graft reduce alveolar-bone resorption and contribute to a significant maintenance of the immediate post-extraction volume and contour of the alveolar crest. But we also found that it was not yet possible to identify the best form of bone graft – either clinically or histologically – because evidence from research that directly compares allografts and xenografts is very limited.
Another critical component in ARP procedures is the sealing of the socket with a barrier to stabilise the blood clot. Several socket-sealing materials have been utilised in ARP procedures. In some situations, soft-tissue conditioning is also needed, and the use of autologous free gingival grafts (FGG; soft-tissue punch) from the palate has been proposed. However, such grafting procedures are technique-sensitivw; so other materials, such as collagen membranes and collagen sponges, have also been evaluated. To date, as in the case of bone grafts, evidence to support the superiority of one socket-sealing material over the others in relation to hard-tissue changes is weak.
To try to better understand the effectiveness of different materials in ARP procedures, we evaluated the efficacy of different techniques based on clinical measurements. The research was led by assistant professor Yiorgos Bobetsis, programme co-director Spyridon Vassilopoulos, and programme director Professor Phoebus Madianos.
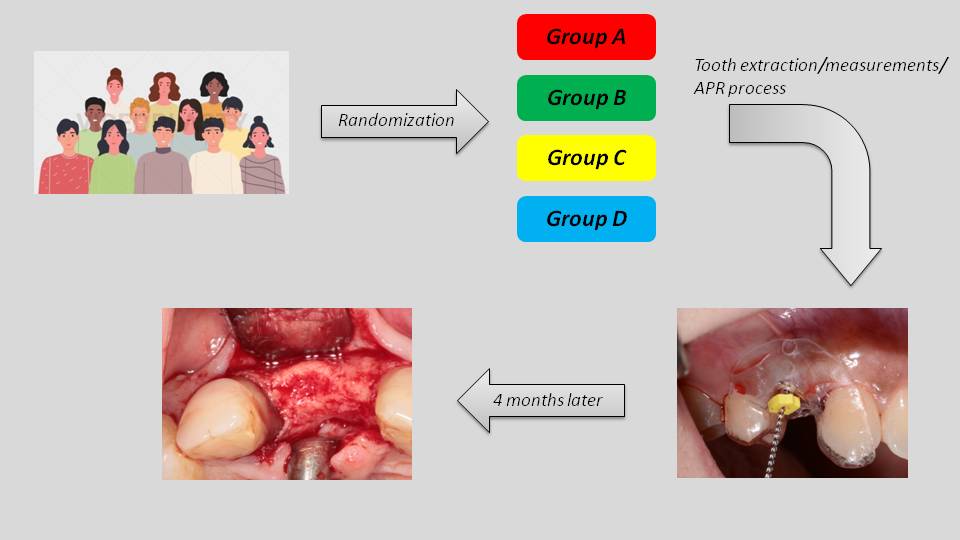
Four treatment groups
In our study, forty-one patients were randomly assigned to four treatment groups:
- Freeze-dried bone allograft (FDBA) covered with collagen sponge (CS).
- FDBA covered with free gingival graft (FGG).
- Demineralised bovine bone mineral xenograft (DBBM) covered with FGG.
- FGG alone.
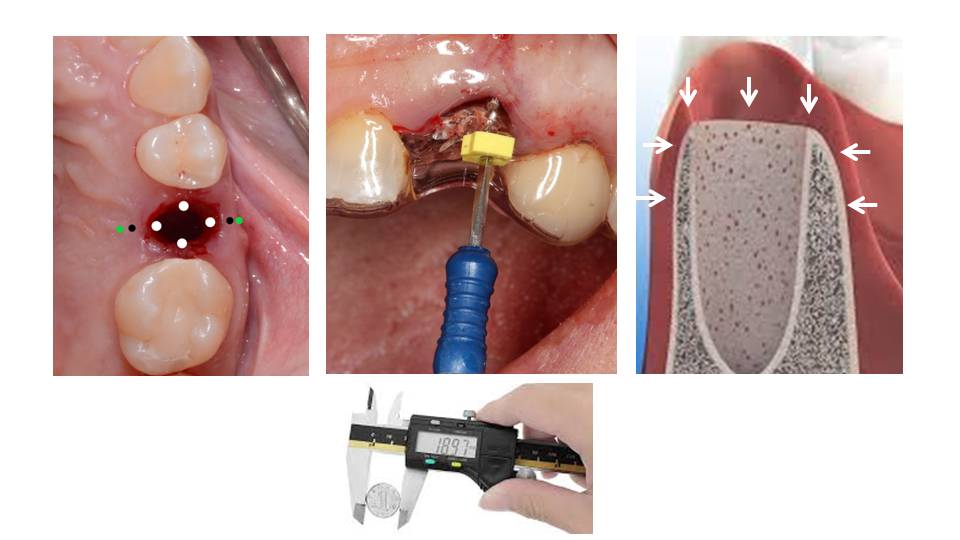
Clinical measurements – assessment of both vertical and horizontal bone loss – were performed immediately after tooth extraction, using surgical stents. Four holes were prepared at the occlusal aspect of the stent: one central-buccal, one mesial, one distal, and one central-lingual above the post-extraction socket. These served as reference points to measure the vertical dimensional alterations after the extraction. In addition, two holes were created at the buccal and two at the lingual aspect of the alveolar ridge (2mm and 4mm apical to the bone margin of the socket) to measure the horizontal dimensional changes of the alveolar ridge.
Four months after tooth extraction, a full-thickness flap was elevated at the site of extraction and, before implant placement, the alveolar-ridge dimensions were measured using the same surgical stents.
Results
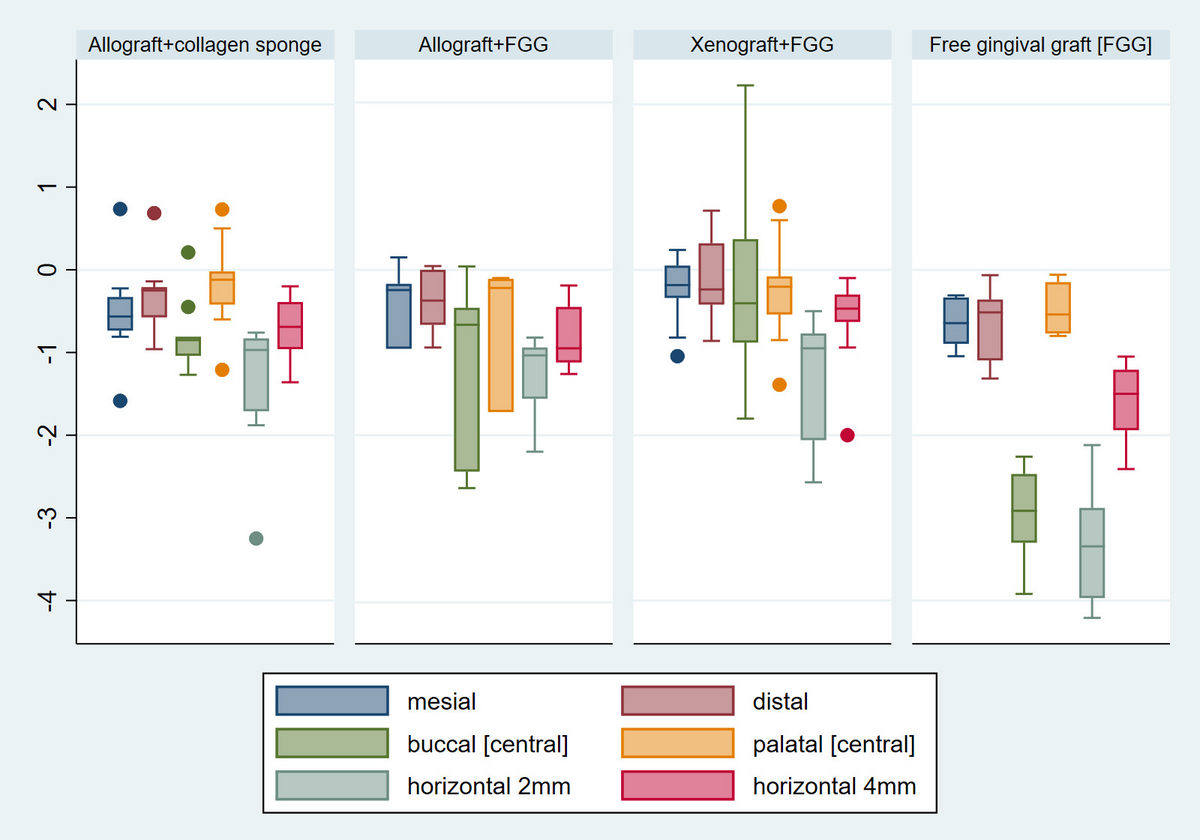
Overall, groups A, B, and C presented significantly less vertical and horizontal bone resorption compared to group D.
In terms of vertical measurements, a common observation across all groups was that greater bone resorption took place at the central buccal region of the alveolar ridge. The median value of bone resorption at the central buccal site was:
- Group A: 0.85mm (interquartile range, IQR: 0.81, 1.04).
- Group B: 0.66mm (IQR: 0.46, 2.44).
- Group C: 0.40mm (IQR: 0.37, 0.88).
- Group D: 2.92mm (IQR: 2.47, 3.30).
Regarding the horizontal level, bone resorption was more pronounced at the 2mm reference point than at the 4mm reference point. Width reduction, at 2mm and 4mm respectively, was:
- Group A: 0.97mm (IQR: 0.83, 1.71) and 0.69mm (IQR: 0.39, 0.96).
- Group B: 1.03mm (IQR: 0.94, 1.56) and 0.95mm (IQR: 0.45, 1.12).
- Group C: 0.95mm (IQR: 0.77, 2.06) and 0.47mm (IQR: 0.30, 0.63).
- Group D: 3.35mm (IQR: 2.88, 3.97) and 1.50mm (IQR: 1.21, 1.94).
The descriptive statistics are summarized and visualized using box plots in Figure 2.
Group B was set as the reference group for all inter-group comparisons. At the vertical level, there was strong evidence of association between bone loss and type of intervention provided at the buccal central region after adjusting for age and tooth type. Specifically, sockets that received solely a FGG (group D) exhibited an increased bone loss of 1.8mm, compared to sockets that also received an allograft (group B): group D vs group B: adjusted β= -1.80 mm; 95%CI: -2.66, -0.94; p<0.001.
On the contrary, sockets that received a xenograft in addition to FGG demonstrated less bone reduction compared to group B, albeit at a marginally significant level (adjusted β: 1.07 mm; 95% CI: 0.01, 2.10; p=0.05). No statistically significant differences were observed between group A and group B. Similarly, no differences were noticed at the mesial, distal, and palatal sites examined.
At the horizontal level, bone resorption was more pronounced at the 2mm level in all groups. Sockets in group D presented significantly greater bone loss compared to group B at the 2mm level (adjusted β= -2.10; 95% CI: -2.77, -1.43; p<0.001), as well as at the 4mm level (adjusted β= -0.80; 95% CI: -1.23, -0.38; p<0.001). No significant differences were detected at the horizontal level between group B and the remaining groups. The effect of age and tooth type was non-significant for all associations under examination.
Our RCT was unable to indicate the superiority of a specific bone-graft material in ARP, except for the mid-buccal site where xenograft was marginally more effective in bone preservation.
One interesting observation in our results was that the collagen sponge as a socket-sealing material was equally effective as FFG in terms of hard-tissue preservation. This result could be explained by the fact that even if the sponge is resorbed rapidly after its placement, it contributes effectively to blood-clot stabilisation and therefore to the stabilization of the bone graft.
Spyridon Vassilopoulos adds: Our study could add some interesting data in the literature regarding ARP techniques and the benefits of these procedures. Of course, there are some drawbacks to be discussed and some open questions we could examine in the future – such as the role of collagen sponge on soft-tissue alterations compared to FFG.
This article is based on ‘Clinical evaluation of different alveolar ridge preservation techniques after tooth extraction: a randomised clinical trial’, Clinical Oral Investigations 27, 4471-4480 (2023). https://doi.org/10.1007/s00784-023-05068-1
Bibliography
Schropp, L., et al., ‘Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study’.Int J Periodontics Restorative Dent, 2003. 23(4), 313-23.
Tan, W.L., et al., ‘A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans’.Clin Oral Implants Res, 2012. 23 Suppl 5, 1-21.
Vignoletti, F., et al., ‘Surgical protocols for ridge preservation after tooth extraction. A systematic review’. Clin Oral Implants Res, 2012. 23 Suppl 5, 22-38.
Avila-Ortiz, G., Chambrone L., and Vignoletti F., ‘Effect of alveolar ridge preservation interventions following tooth extraction: A systematic review and meta-analysis’.J Clin Periodontol, 2019. 46 Suppl 21: p. 195-223.
Tonetti, M.S., et al., ‘Management of the extraction socket and timing of implant placement: Consensus report and clinical recommendations of group 3 of the XV European Workshop in Periodontology’.J Clin Periodontol, 2019. 46 Suppl 21, 83-194.
Kim, Y.K., et al., ‘Ridge preservation of the molar extraction socket using collagen sponge and xenogeneic bone grafts’.Implant Dent, 2011. 20(4), 267-72.
Karaca, C., et al., ‘Alveolar ridge preservation with a free gingival graft in the anterior maxilla: volumetric evaluation in a randomized clinical trial’.Int J Oral Maxillofac Surg, 2015. 44(6), 774-80.
Biography

Iosif El Sioufi graduated from the Dental School of the National and Kapodistrian University of Athens in 2013. Early in his undergraduate studies, he realised that periodontology was the speciality he wanted to dedicate himself to. He completed the full-time EFP-accredited three-year programme in periodontology at the National and Kapodistrian University, where he is now a clinical instructor in the Department of Periodontology. He also has a private practice.