Therapy
Adjacent teeth have no impact on marginal bone levels around implants
30 July 2024
In the final of a series of articles by the four winners of the EFP Graduate Research Prize 2023, Lucienne Weigel (University of Bern, Switzerland) describes a retrospective study into marginal bone level changes around dental implants.
Does the presence of one or two adjacent teeth have an impact on marginal bone level changes around implants?
This was the question that our retrospective study set out to investigate, working from the hypothesis that the periodontal attachment of a tooth adjacent to a dental implant would play a beneficial role in maintaining the peri-implant marginal bone level.
Although dental implants have become a highly successful therapeutic choice to replace missing teeth with high long-term survival rates (95% after 10 years), periodontally compromised patients have been shown to be at higher risk for implant loss. In this context, it might be tempting in some patients with teeth with a doubtful prognosis to proceed to extraction and implant placement.
However, the more implants a patient has, the greater the risk of peri-implantitis developing.
When considering crestal/marginal bone level changes comparing periodontally compromised teeth with implants, little long-term evidence is available. The hypothesis behind our study was that the periodontal attachment of a tooth adjacent to a dental implant plays a beneficial role in maintaining the peri-implant marginal bone level. Given the paucity of data on this topic, the aim of this retrospective comparative study was to compare mean bone level (mBL) changes around dental implants with one or two adjacent teeth after at least 10 years of supportive periodontal care (SPC).
The study involved two groups of patients – those with a mesial and distal adjacent tooth (tooth-implant-tooth, or TIT) and those with an implant with only one mesial or distal adjacent tooth and a gap or free-end situation (tooth-implant-gap, or TIG). Data was analysed from 87 patients who underwent implant placement up to September 2011 at the Department of Periodontology, University of Bern, Switzerland. Sixty-one implants (43%) were categorized as TIT and 81 (57%) as TIG.
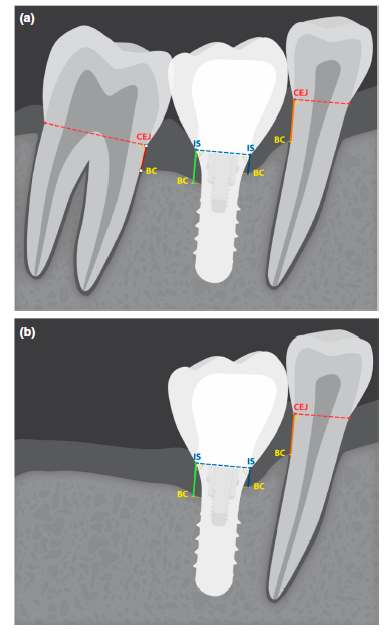
Four different comparisons between baseline (T0) and the follow-up of at least 10 years later (T1) were performed with radiographic analysis:
- mBL change on the mesial implant surface in TIT group and mesial implant surface without adjacent tooth in TIG group (Figure 1, blue line).
- mBL change on the distal implant surface in the TIT and distal implant surface without adjacent tooth in TIG group (green line).
- mBL change at tooth site facing the mesial implant surface in TIT group and facing the mesial implant surface in TIG group (orange line).
- mBL change at tooth site facing the distal implant surface in TIT group and facing the distal implant surface in TIG group (red line).
At T0 there were no statistically different bone level measurements between the two groups for the mesial and distal implant sites. At T1, the results included:
- Mesial implant site: At T1: TIT group: mBL 0.13 ± 1.07mm; TIG group: mBL 0.99 ± 1.86mm (statistically significant difference, 95% CI: 0.16/1.56, p = .016). While the mBL increased in the TIT group (T1–T0: −0.07 ± 0.92mm), it decreased in group TIG (T1–T0: 0.52 ± 1.34mm), with a statistically significant difference (95% CI: 0.04/1.14, p = .037).
- Distal implant site: no statistical differences over time between the two groups (T1–T0: 95% CI: −0.20/0.42, p = .482).
- Teeth adjacent to the mesial implant site: TIT group, slight decrease from 3.7 ± 1.63mm to 3.94 ± 1.5 mm (T1–T0:0.24 ± 1.29mm); TIG group a decrease from 3.81 ± 1.63 mm to 4.21 ± 1.69mm (T1–T0: 0.48 ± 1.15mm) with no statistically significant difference between the two groups (95% CI: −0.20/0.68, p = .285).
- Comparing the teeth adjacent to the distal site of the implant, a statistically significant difference between the TIT and TIG groups at T0 was calculated (95% CI: −1.37/−0.01, p = .049), but at T1 no statistically significant difference between the groups could be measured.
The overall implant loss rate was 3.5% (2 TIT, 3 TIG), with no statistically significant difference between the two groups. In terms of tooth loss in the TIT group, 13 patients (15 implants) lost one adjacent tooth (24.6%), while in the TIG group 10 patients (10 implants) lost one adjacent tooth (12.3%). With respect to the total number of adjacent teeth, the rate of tooth loss (i.e., 12.3%) was not statistically significantly different between the two groups.
Hypothesis rejected
Our study indicated high survival rates for both teeth (87.7%) and implants (96.5%) and there was a similar survival rate between implants with two adjacent teeth (96.7%) and those with one adjacent tooth (96.3%).
Although all patients in the study had a history of periodontal disease – well documented as a risk factor for developing peri-implant diseases – only 7.7% of implants underwent surgical interventions to treat peri-implantitis. It seems likely that this low rate is related to the high level of compliance by patients with a tailored supportive periodontal care programme.
Our research was based on the scientific hypothesis that periodontal attachment of a tooth adjacent to a dental implant plays a beneficial role in maintaining the peri-implant marginal bone level. But the results obtained led us to reject this hypothesis because comparable peri-implant marginal bone level changes were observed at both the implant sites with and without adjacent teeth.
This article is based on Weigel, L. D., Scherrer, A., Schmid, L., Stähli, A., Imber, J.-C., Roccuzzo, A., & Salvi, G. E. (2023). Marginal bone level changes around dental implants with one or two adjacent teeth – A clinical and radiographic retrospective study with a follow-up of at least 10 years. Clinical Oral Implants Research, 34, 872–880. https://doi. org/10.1111/clr.14115.
Note: The EFP Graduate Research Prize seeks to promote original graduate research, performed within the framework of postgraduate training the federation’s accredited graduate programmes in periodontology. It is awarded annually in two categories: clinical research and preclinical/basic research. It is open to all students of EFP accredited graduate programmes in periodontology.
Bibliography
Carra, M. C., Range, H., Swerts, P. J., Tuand, K., Vandamme, K., & Bouchard, P. (2022). Effectiveness of implant-supported fixed partial denture in patients with history of periodontitis: A systematic review and meta-analysis. Journal of Clinical Periodontology, 49(Suppl 24), 208–223. https://doi.org/10.1111/jcpe.13481
Rasperini, G., Siciliano, V. I., Cafiero, C., Salvi, G. E., Blasi, A., & Aglietta, M. (2014). Crestal bone changes at teeth and implants in periodontally healthy and periodontally compromised patients. A 10-year comparative case-series study. Journal of Periodontology, 85(6), e152–e159. https://doi.org/10.1902/jop.2013.130415
Roccuzzo, A., Imber, J. C., Marruganti, C., Salvi, G. E., Ramieri, G., & Roccuzzo, M. (2022). Clinical outcomes of dental implants in patients with and without history of periodontitis: A 20-year prospective study. Journal of Clinical Periodontology, 49, 1346–1356. https://doi.org/10.1111/jcpe.13716

Biography
Lucienne Weigel graduated in dentistry from the University of Bern, Switzerland. She holds a Doctor Medicinae Dentium (Dr. med. dent.) and a master’s degree in periodontology and implant dentistry from the same institution. She is a specialist in periodontology (EFP) after completing the EFP-accredited postgraduate programme in periodontology and implant dentistry at the University of Bern.