Prevention & Public health
Women and oral health: views from periodontology and gynaecology
20 December 2023
Hormonal changes have a complex influence on women's gum health, with alterations in hormonal balance occurring at puberty, the menstrual cycle, contraceptive use, pregnancy, in vitro fertilisation (IVF), and post-menopause. Gynaecologist Renée Behrens and periodontist Ali Çekici – who recently participated in an EFP Perio Talks podcast on women’s oral health – explore the issues.
Renée Behrens: How hormonal milieu may affect a woman’s susceptibility to periodontal disease
There is an increasing realisation of the impact of the human biome on health and disease, and the oral cavity is one of the densest microbial environments in the body. Despite this, there remains a lack of understanding regarding oral health and disease and the possible contribution of female hormones.
Across a diverse range of cultures women appear to have a higher incidence of dental caries.1 The underlying risk factors have been postulated to include the earlier eruption of permanent dentition in girls (and therefore longer exposure to cariogenic risk), the differing diets of women and men, and pregnancy. Pregnancy has long been thought to be a major risk factor for gingivitis and caries, but there is uncertainty about the underlying causes. This raises the question of the impact of female hormones on oral health.
At puberty, girls start to experience the production of oestrogen and, later, progesterone from ovarian egg development. This continues throughout their reproductive life with the menstrual cycle and with the use of hormonal contraceptives. In vitro fertilisation protocols utilise high levels of gonadotrophins to allow the development of multiple eggs, each of which produces oestrogen. This results in super-ovulation and correspondingly elevated levels of oestrogen for the three to four weeks of treatment. But it is pregnancy that remains the time associated with the highest levels of both oestrogen and progesterone, and it has long been thought to be associated with an increased risk of both dental caries and gingivitis.
During pregnancy, progesterone is the dominant hormone required for implantation, maintenance of pregnancy, and the suppression of pre-term labour. Progesterone also acts to supress the maternal immunologic response, important in preventing maternal rejection of ‘foreign’ foetal antigens. This reduction in natural immunity during pregnancy means that pregnancy is a period of relative immunosuppression and there is greater morbidity and risk of death from infections including influenza A and SARS-CoV-2. This reduction in natural immunity may increase susceptibility to bacterial infection and there have been some studies showing an increase in cariogenic strains of bacteria during pregnancy.
There is a growing body of evidence that oestrogen is associated with a higher incidence of caries whereas androgens (male hormones) are not. Receptors for both oestrogen and progesterone have been shown in the salivary glands and gingival tissue,2, 3 indicating that these tissues respond to hormonal influence. Oestrogen has been demonstrated to affect both the composition – with a reduction in buffering capacity – and the flow rate of saliva, thus predisposing to increased bacterial growth and caries.
More recently, there is a growing understanding that poor oral health and active gingivitis in pregnant women is associated with an increased risk for pre-term and low-birth-weight babies, as well as the development of high blood pressure (pre-eclampsia) during pregnancy. Bacteria originating from the oral cavity have been found in the placenta and in the amniotic fluid surrounding the baby.
In summary, the hormonal milieu appears to affect a woman’s susceptibility to periodontal disease with a particular risk around the time of pregnancy. The higher incidence of caries in women implicates an impact of endogenous sex-steroid hormones on oral health at puberty, menstruation, pregnancy, menopause, and with the use of the contraceptive pills and hormone-replacement therapy. These factors are important for understanding and manipulating oral health and disease in women.
However, there is evidence that maintaining good oral hygiene and plaque control can mitigate the impact and risks of hormonal fluctuation, and a greater understanding of this by both women and medical professionals will improve outcomes.
References
1. Lukacs JR, Largaespada LL. Explaining sex differences in dental caries prevalence: saliva, hormones, and "life-history" etiologies. Am J Hum Biol. 2006 Jul-Aug;18(4):540-55. doi: 10.1002/ajhb.20530. PMID: 16788889.
2. Vittek J, Munnangi PR, Gordon GG, Rappaport S, Southren AL. Progesterone “receptors” in human gingiva. IRCS Med Sci 1982: 10: 381–384.
3. Vittek J, Hernendez MR, Wennk EJ, Rappaport SC, Southren AL. Specific estrogen receptors in human gingiva. J Clin Endocrinol Metab 1982: 54: 608–612.
Ali Çekici: The role of sex hormones on periodontal tissues at the key stages of a woman’s life

At certain stages in a women’s life, sex hormones affect oral tissues. Gingival epithelial cells have oestrogen receptors and can detect changing oestrogen levels. They are one of the first cells in defence that respond earliest to bacterial infection. During certain periods in a women’s lifetime when sex hormones fluctuate – such as adolescence, pregnancy, menopause, and post-menopause – it is possible to experience some adverse clinical symptoms in tooth-surrounding tissues that would affect a person’s life quality. Periodontal health, referring to the well-being of the tissues surrounding and supporting the teeth, plays a pivotal role in overall health and its connections with women's health are becoming increasingly apparent.
Menstrual cycle:
Studies suggest that women may experience variations in gum health across their menstrual cycle. During menstruation, some women may observe increased gingival inflammation, bleeding, or discomfort. Understanding these cyclic variations is essential for tailored oral-health care, emphasising the importance of regular dental check-ups and preventive measures.
Pregnancy and periodontal health:
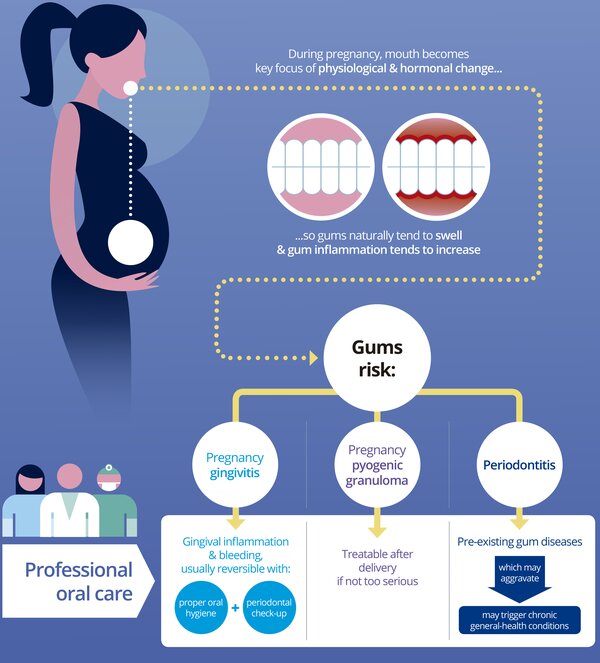
Pregnancy introduces a unique set of challenges and considerations for women's health, and periodontal health is no exception. Research indicates a potential link between periodontal disease and adverse pregnancy outcomes, including preterm birth and low birth weight. Hormonal changes during pregnancy can intensify the body's response to oral bacteria in the dental plaque biofilm, underscoring the need for heightened oral-hygiene practices and professional dental care during this crucial period. If a women’s tooth-surrounding tissues are not healthy before pregnancy, then the risk of having severe gingival inflammation and gingival enlargement is much more likely to be experienced.
Menopause and post-menopause:
As women transition through menopause, hormonal fluctuations continue to influence periodontal health. The decline in oestrogen levels may contribute to changes in oral tissues, potentially leading to increased susceptibility to periodontal disease. Maintaining regular dental check-ups and a personalised oral-hygiene routine will increase quality of life and improve oral health.
IVF and freezing eggs:
IVF (in vitro fertilization) and freezing-eggs treatments also include medical procedures that change women's hormonal balance. The same medical procedure is applied in these two medical practices: women are essentially given medications to make them produce more hormones. If the person receiving this treatment has a healthy mouth before and the treatment does not last very long, it will not have serious effects on oral health.
Empowerment:
Empowering women with knowledge about these connections and encouraging regular dental care will contribute not only to optimal periodontal health but also overall well-being throughout the various stages of a woman's life.
References:
Smith, A. et al. (2010). The Impact of Estrogen on Gingival Tissues. Journal of Dental Research, 89(5), 432-438.
Smith, J. (2020). The Hormonal Impact on Oral Health. Journal of Dental Research, 45(2), 123-135.
Zeeman GG. et al. (2001). Focus on primary care: periodontal disease: implications for women's health. Obstet Gynecol Surv. 56(1): 43-9.
EFP campaign, Oral Health & Pregnancy, https://www.efp.org/for-patients/gum-disease-general-health/oral-health-pregnancy/.

Biographies
Renée Behrens is a consultant gynaecologist in Winchester, UK. Her areas of specialist interest include early pregnancy complications, recurrent miscarriage, and fertility. She is the lead for gynaecology at the Hampshire and Isle of Wight Integrated Care Board, which comprises four Hospital trusts serving the South East of England. Originally from Jamaica, Renée completed medical training at the University of the West Indies and post-graduate training in London and was awarded an MD for research into Polycystic Ovarian Syndrome and embryo implantation. She speaks locally and nationally and is involved in training the next generation of doctors.

Ali Çekici is an associate professor at the Istanbul University Dental Faculty Department of Periodontology in Turkey. He completed his two-year post-doctoral research at The Forsyth Institute in Boston, USA. His areas of professional interest are the effects of sex hormones on periodontal tissues, periodontal immunology, non-surgical periodontal therapy, periodontal plastic surgery and dental implants. He has been awarded by the IADR for his work on the effects of hormone replacement therapy on periodontal tissues in post-menopausal women.
He has been a board member of the Turkish Society of Periodontology since 2014, where he still serves as the general secretary. He is also a member of the EFP Scientific Affairs Committee.